Frequency of Metabolic Syndrome in Type 2 Diabetes Mellitus in a Tertiary Care Hospital of Bangladesh
CURRENT RESEARCH IN DIABETES & OBESITY JOURNAL JUNIPER PUBLISHERS
Authored by MSI Tipu Chowdhury
Abstract
Background: As a well-established risk factor for coronary heart disease, Metabolic Syndrome was already encountered. But the relationship between Metabolic Syndrome and Type 2 Diabetes Mellitus and independent contribution of Metabolic Syndrome remained unclear. To evaluate the status of metabolic syndrome in Type 2 diabetic population and for their ability to predict Type 2 Diabetes Mellitus, in parallel with conventional stroke risk factors, this study was planned.
Methods: A hospital based descriptive observational study was conducted in 100 patients with Type 2 Diabetes Mellitus who were selected by consecutive random sampling technique. Patients were diagnosed through proper history, clinical examination and necessary investigations. The outcome values were measured in the form of anthropometric measurements, blood pressure, dyslipidemia and blood glucose.
Results: Among 100 patients of Type 2 Diabetes Mellitus 64 (64%) were female who were housewife (41%) with significant difference (p < 0.001) and Mean±SD was 58±12.24 yrs ranging from 32-85 years. About 30% had a positive family history of Type 2 Diabetes Mellitus and 28% tobacco abuse. Of the total, 31% patients had high blood pressure and 28% had low HDL with a significant difference (p<0.001) but 46% had high triglyceride level which was not significant. More than half (53.12%) female showed central obesity, while among male only 16.67% had central obesity and it showed significant difference (p=0.04) in both sex. There was a high frequency of Metabolic Syndrome in patient with Type 2 Diabetes Mellitus (68%) with significant difference and 48% were female and 20 % were male. In patients of Metabolic Syndrome, central obesity found in 36(52.94%) patients where female was predominantly affected 32(88.89%), hypertension found in 28(4118%) patients where male was predominantly affected 16(57.14%) patients, hyper-triglyceridemia found in 44(64.70%) patients where female was predominantly affected 26(59.09%) patients and low HDL found in 22(32.35%) patients where female was predominantly affected 16(72.73%).
Conclusion: The frequency of Metabolic Syndrome was more than double in women (48%), central obesity and low HDL was significantly more prevalent in women compared to men where hypertension was significant in men. So, it would be reasonable to conclude that women are more likely to suffer from Metabolic Syndrome that is from cardiovascular morbidity and mortality.
Keywords: Metabolic syndrome; Central obesity; Waist-Hip Ratio; Blood pressure; Dyslipidemia
Abbreviations: LDL: Low-Density Lipoprotein; VLDL: Very Low-Density Lipoprotein; BMI: Body Mass Index; WC: Waist Circumference; WHR: Waist-Hip Ratio; FPG: Fasting Plasma Glucose; OGTT: Oral Glucose Tolerance Test; DCCT: Diabetes Control and Complications Trial; NGSP: National Glycohemoglobin Standardization Program; SPSS: Statistical Package for Social Science
Introduction
Metabolic Syndrome is major health problem globally and it increases various cardiovascular disease risk factors like diabetes and pre-diabetes, abdominal obesity, hyperlipidaemia and high blood pressure. People with Metabolic Syndrome have a five-fold greater risk of developing Type 2 Diabetes Mellitus [1]. There is several definitions for the Metabolic Syndrome. The National Cholesterol Education Program (NCEP/ATP III) and International Diabetes Federation (IDF) definitions are the most widely used [2]. It is now believed that Metabolic Syndrome is driving the twin global epidemics of Type 2 Diabetes and cardiovascular disease. South Asians have high prevalence of Metabolic Syndrome [3] and an unusually high tendency to develop Type 2 Diabetes Mellitus and atherosclerotic cardiovascular disease (ASCVD) [4]. In order to reduce the medical and economic burdens, it is imperative to identify patients of Metabolic Syndrome and treat them early with lifestyle modification and drugs, where needed.
Obesity, particularly abdominal obesity, is associated with resistance to the effects of insulin on peripheral glucose and fatty acid utilization, often leading to Type 2 Diabetes Mellitus. Insulin resistance, the associated hyperinsulinemia and hyperglycaemia, and adipocyte cytokines (adipokines) may also lead to vascular endothelial dysfunction, an abnormal lipid profile, hypertension, and vascular inflammation, all of which promote the development of atherosclerotic cardiovascular disease (ASCVD) [5]. A similar profile can be seen in individuals with abdominal obesity who do not have an excess of total body weight [6].
Obesity is strongly associated with reduced longevity as well as with stroke, diabetes, thrombosis, and the development of coronary artery disease. Obesity contributes to the development of atherosclerosis and transition to the acute ischemic stroke [7]. Obesity leads to insulin resistance that, in turn, leads to a cluster of traditional risk factors, known as the metabolic syndrome, which facilitates atherogenesis [8]. Increased intraabdominal fat causes ‘central’ (‘abdominal’, ‘visceral’, ‘android’ or ‘apple-shaped’) obesity, which contrasts with subcutaneous fat accumulation causing ‘generalized’ (‘gynoid’ or ‘pear-shaped’) obesity; the former is more common in men and is more closely associated with Type 2 Diabetes, the Metabolic Syndrome and cardiovascular disease and ischemic stroke as well. Abdominal obesity is an independent, potent risk factor for ischemic stroke in all race & ethnic groups. It is a stronger risk factor than BMI and has a greater effect on younger persons [9].
In insulin-resistant individuals, the adipose tissues have a diminished capacity to take up free fatty acids. These free fatty acids are available to the liver that, as a result, secretes an increased amount of very low-density lipoprotein (VLDL) [10]. VLDL delivers cholesterol to the vessel wall facilitating atherogenesis. Also, in insulin-resistant individuals, the highdensity lipoprotein (HDL) cholesterol concentration is reduced and dense low-density lipoprotein (LDL) cholesterol particles are generated [9].
Body mass index (BMI) is altered by parameters other than body fat, such as muscle mass and fluid status. Abdominal obesity, measured by waist circumference (WC) or waist-hip ratio (WHR), has been suggested as a better predictor of cardiovascular and stroke events [11]. Obesity can be measured by BMI, waist circumference (WC) and waist-hip ratio (WHR). WHR may be preferred measures of the ischemic stroke risk associated with obesity. In contrast with BMI, WHR specifically address abdominal obesity and correlate better with overall atherosclerotic disease prevalence. WHR is obtained by dividing the mean waist circumference (measured between the lower border of the ribs, and the iliac crest in a horizontal plane) by the mean hipcircumference (measured at the widest point over the buttocks). Abdominal obesity, measured by waist circumference or WHR, has been suggested as a better predictor for cardiovascular risk [12].
People with metabolic syndrome are twice as likely to die from and three times as likely to have a heart attack compared with people without the syndrome. Studies have shown that Asians have higher percentage of adiposity at lower BMI than Caucasians and are more prone to develop Metabolic Syndrome. Obesity, particularly abdominal obesity, is associated with resistance to the effects of insulin on peripheral glucose and fatty acid utilization, often leading to Type 2 Diabetes Mellitus and type-2 diabetes mellitus patients are more prone to develop Metabolic Syndrome. But there is no data available regarding actual number of people affected in Bangladesh. So, the present study aimed to observe the status of Metabolic Syndrome in Type 2 Diabetes Mellitus patients, to describe patients of metabolic syndrome, to observe the clustering of cardiovascular risk factor in Type 2 Diabetes Mellitus and to observe the demographic profile.
Materials and Methodology
This hospital based descriptive type of observational study was carried out at Dhaka Medical College and Hospital (DMCH, Dhaka, Bangladesh, October 2012 to April 2013 after getting ethical clearance from ERC (Ethical Review Committee) of DMCH. The sample was selected by purposive sampling technique. Though calculated sample size was 96 but a total of 100 samples taken in the study.
Inclusion criteria
a) Patients of diagnosed type 2 diabetes mellitus.
b) Age- more than 30 years.
Exclusion criteria
a. Patients with acute illness. (e.g. Stroke, myocardial infarction)
b. Patients with other co-morbidity. (e.g. genetic or congenital defect in height and weight, ascites, pregnancy)
c. Patients on regular anti-dyslipidemic drugs, diuretics and beta blocker.
Data collection procedure
After arrival of a patient of known Type2 Diabetes Mellitus, immediately attend the patient and examine thoroughly to measure weight (kg), height and waist circumference (centemeters) and then BMI was calculated. Pulse and BP was recorded. The CRF was filled by the study physician herself by direct face to face interview method. Then about 5 ml of blood was collected for estimation of FBS and fasting lipid profile (total cholesterol, LDL, HDL, TG.). Spot collection of samples at outdoor and sample collection was done within 24 hrs for indoor patients. Those patients at outdoor were not in fasting state was asked to come on next morning at fasting state. The sample was sent to the pathology department of DMCH and these were analyzed by automated analyzer machine Biolis24i machine. Patients were enrolled in the study after briefed about the objectives, risk and benefits, freedom for participating in the study and confidentiality. Informed consent was obtained accordingly. The pre structured CRF was filled up by the study physician himself.
Diagnostic tools
Diagnostic criteria of diabetes mellitus: A diagnosis of diabetes, as defined by the American Diabetes Association (ADA), requires one of the following four criteria to be met:
a. Fasting plasma glucose (FPG): 126mg/l (7.0 mmol/L) after a minimum of eight hours with no caloric intake,
b. Symptoms of hyperglycemia and a casual (random) plasma glucose: 200 mg/dL (11.1 mmol/L),
c. Two hours plasma glucose:00 mg/dl (11.1 mmol/L) during a 75-gram oral glucose tolerance test (OGTT), or
d. Glycated hemoglobin A1c (HbA1c): 6.5% using a method that is National Glycohemoglobin Standardization Program (NGSP) certified and standardized to the Diabetes Control and Complications Trial (DCCT) assay [13].
Anthropometry: The data on anthropometry includes Waist Circumference (WC) and Waist Hip Ratio (WHR). By using standard non-elastic tape, WHR is obtained by dividing the mean waist circumference (measured between the lower border of the ribs, and the iliac crest in a horizontal plane) by the mean hipcircumference (measured at the widest point over the buttocks). WC was measured midway between the iliac crest and costal margins after removing folds of clothing. Standard landmarks and methodology were followed in recording the anthropometric measurements [14].
Operational definitions
a. Hypertension: BP>140/90mmHg or patients on antihypertensive medication (JNC- 7, 2004) [3].
b. Diabetes Mellitus: Symptoms of diabetes plus causal plasma glucose concentration 200mg/dl (11.1mmol/l) or Fasting plasma glucose.126mg/dl (7mmol/l). Type2 Diabetes Mellitus was defined as diabetes mellitus develop after the age of 30 years [4].
c. Body mass index: BMI is calculated in (kg/m2). Classification of overweight and obesity by BMI:
Classification BMI kg/m2
Healthy weight 18.5-24.977
d. Obesity: The recommended BMI cut of value for Asians for overweight are 23-25 kg/m2 [15].
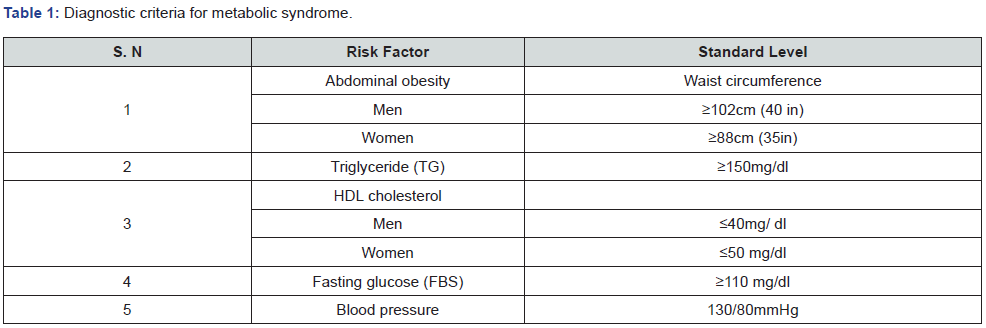
e. Metabolic Syndrome: Diagnostic criteria for metabolic syndrome include 3 or more of the following [16] (Table 1):
f. Waist circumference: It is considered as the intermediate abdominal area, perimeter between the last costal arch and the iliac crest measured. During measurement tape must be kept horizontal [15].
Data analysis
Data was analyzed using computer-based software, statistical package for social science (SPSS) version 15. Continuous variables like age, waist circumference, WHR were calculated as mean standard deviation. Cross tabulation was performed to get the relation between males and females. Categorical variables like gender, history of hypertension, diabetes mellitus, smoking, dyslipidaemia was presented in frequencies and percentages.
Results
One hundred patients of diagnosed Type 2 Diabetes Mellitus patients were studied in Dhaka Medical College Hospital, Dhaka, from July to December 2012. Table 2 shows that majority of patients were female and the Mean±SD of both male and female patients. It was found that about one-third patients with positive family history of Type 2 Diabetes Mellitus and tobacco abuse. Maximum number of Type 2 Diabetes Mellitus patients (about 94%) was above 40 years of age and maximum frequency was found in between 60-69 years (about 29%) (Table 3).
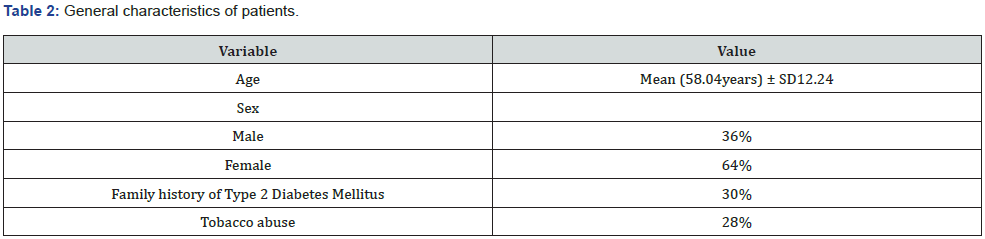
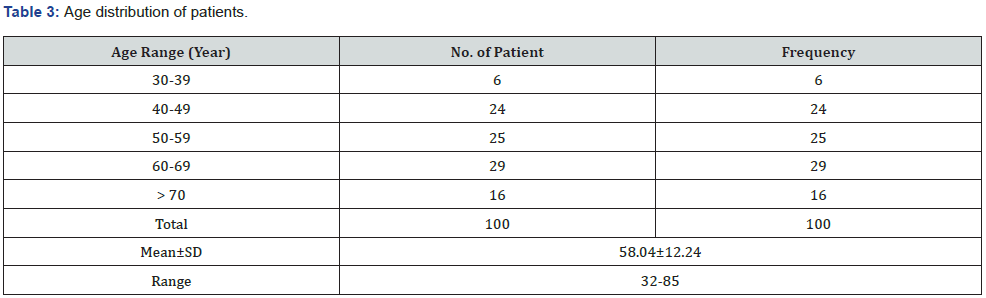
Figure 1 shows that most of the patients were housewife (41%) followed by businessman (22%) and then service holder (20%).
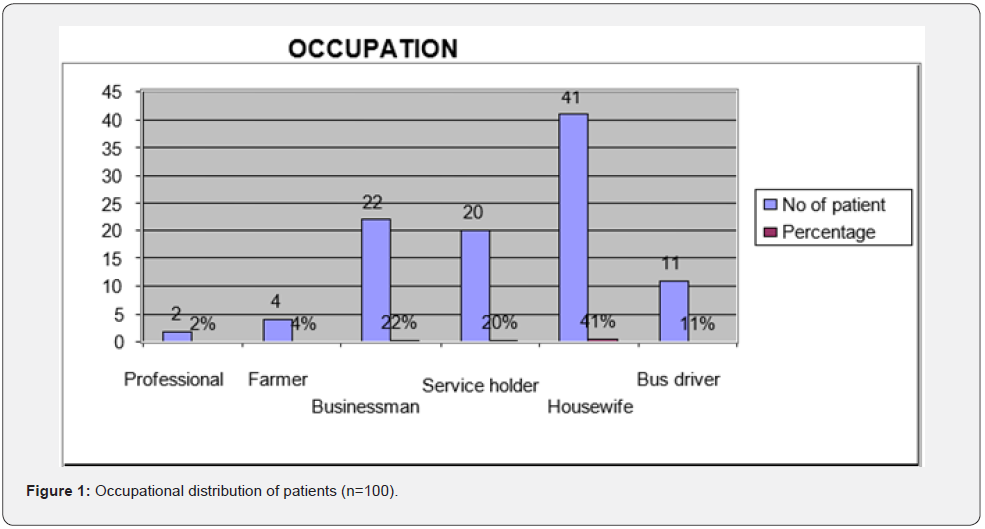
Table 4 shows that majority of the patients belong to 40 years and above (94%) with a female predominance 64(64%).
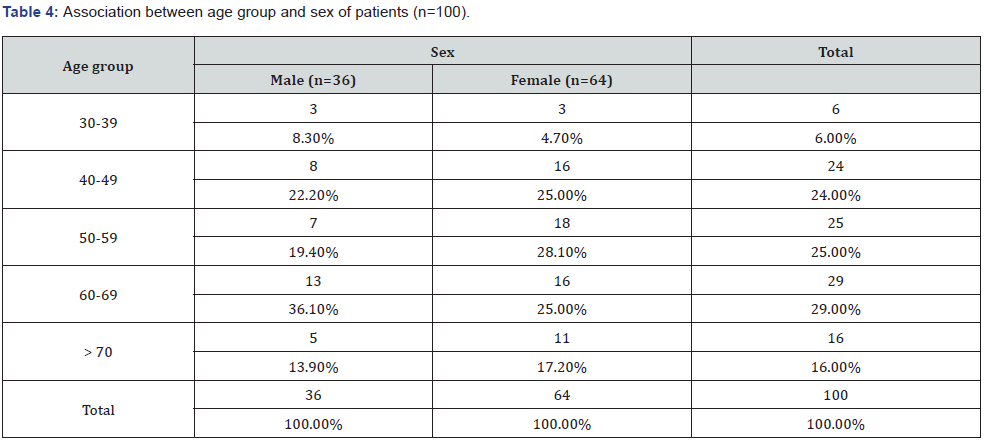
Chi-square test χ2 =2.416 df = 4 p=0.67
Table 5 shows the frequency Metabolic Syndrome with sex. In this study, 68% among Type 2 Diabetes Mellitus patient showed a female predominance (75%) with a significant difference.
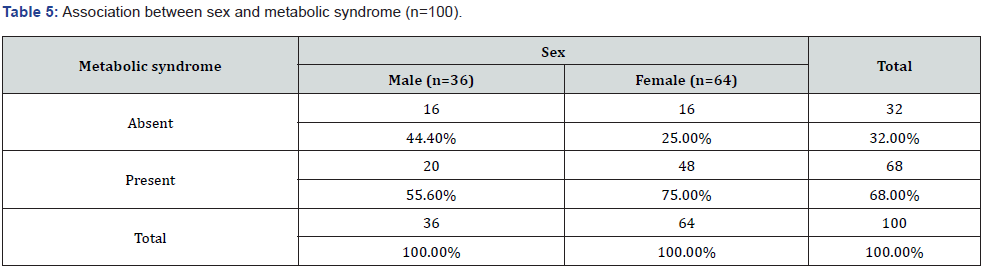
Chi-square test χ2 =4.03, df = 1 p=0.04 (significant)
Central obesity was present in 40% patients of Type 2 Diabetes Mellitus with a female predominance (53.1%) which showed significant difference (Table 6).
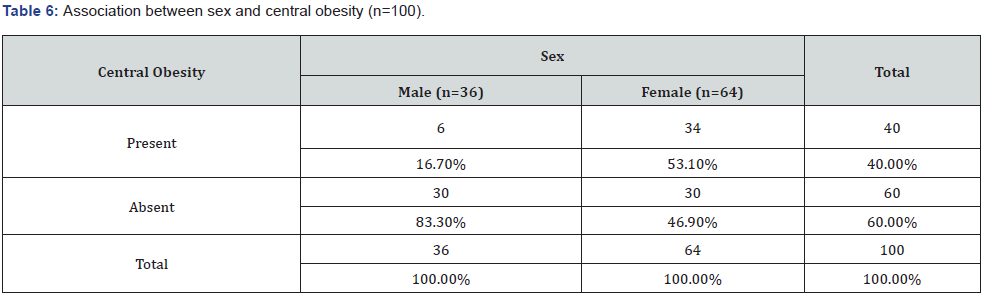
Chi-square test χ2 =12.76, df = 1, p < 0.001 (significant)
Table 7 shows that hypertension present in 31% patients of Type 2 Diabetes Mellitus with a male predominance (55.6%) and significant difference.
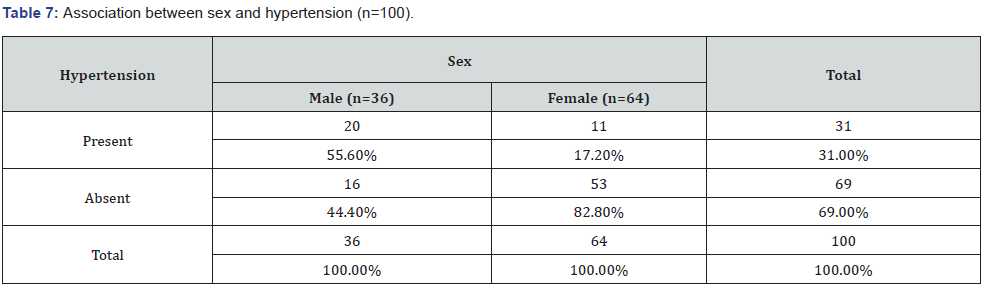
Chi-square test χ2 =15.86 df = 1 p < 0.001 (significant)
A higher triglyceride (TG) was present in 54% patients of Type 2 Diabetes Mellitus with a female predominance (59.4%) (Table 8).
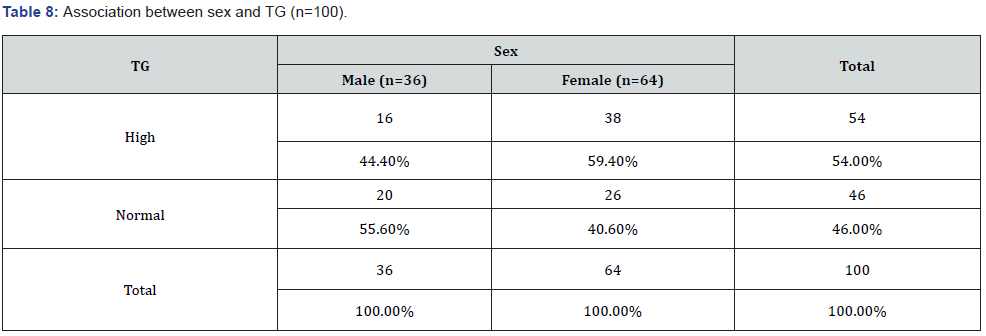
Chi-square test χ2 =2.06 df = 1 p = 0.15
Table 9 shows a low level of HDL present in 28.0% patients of Type 2 Diabetes Mellitus with a female predominance (29.7%).
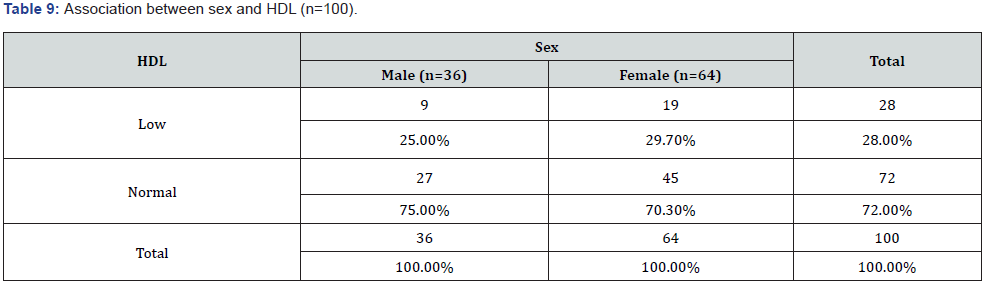
Chi-square test χ2 =0.251, df = 1, p = 0.62
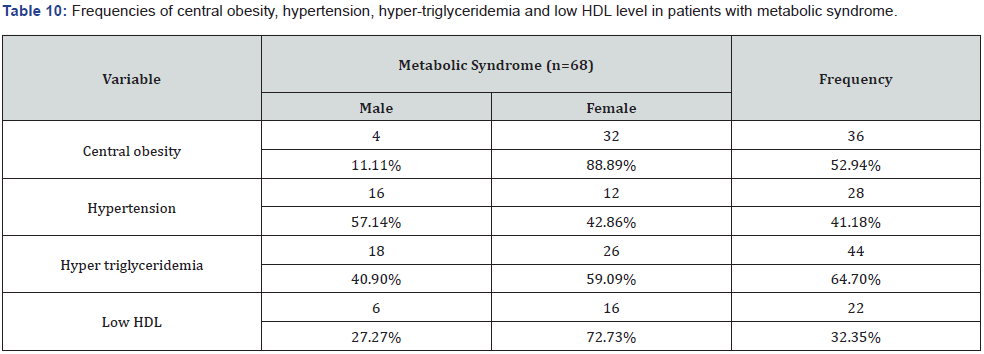
In patients of Metabolic Syndrome, central obesity found in 36(52.94%) patients where female was predominantly affected 32(88.89%), hypertension found in 28(4118%) patients where male were predominantly affected 16(57.14%) patients, hypertriglyceridemia found in 44(64.70%) patients where female was predominantly affected 26(59.09%) patients and low HDL found in 22(32.35%) patients where female was predominantly affected 16(72.73%) (Table 10).
Discussion
This observational descriptive study was done among 100 patients of Type 2 Diabetes Mellitus at Dhaka Medical College Hospital. The frequency Metabolic Syndrome in this study is 68% among Type 2 Diabetes Mellitus patient with a female predominance (75%) which is consistent with a prior study done in the Diabetes Clinic of Nishtar Medical College and Hospital, Multan. In their study, involving a total of 187 Type 2 Diabetic patients in which the frequency Metabolic Syndrome was 65.2% with a female predominance (43.3%) [17]. This finding is also nearer to the study done in Liaquat National Hospital, Karachi among 233 patients with Type 2 Diabetes Mellitus which showed frequency of Metabolic Syndrome was 79.7% with female predominance (45.5%) by applying NCEPATP III criteria and 68.1% Metabolic Syndrome with a female predominance (43.7%) by applying IDF criteria [18]. But these findings are not consistent with a cross sectional study at OPD BIRDEM hospital among 100 DM and 44 IGT subjects in which 39.6% Metabolic Syndrome have present [19].
The main reason of female predominance in Metabolic Syndrome is possibly the high rate of central obesity in female. The frequency of central obesity among the patients of Metabolic Syndrome was 32 (88.89%). This may be related to sedentary lifestyle of women and due to religious and social barriers [20]. In this study most patients are housewife (41%) followed by businessman (22%) who also lead a sedentary lifestyle. Moreover, abdominal obesity is common in south Asians and evident in non-obese people having a high percentage of body fat, thick subcutaneous adipose tissue, low muscle mass, insulin resistance and hyperinsulinaemia. This body composition is conducive to the development of Metabolic Syndrome [21].
In American blacks, Mexican Americans, Korea, Iran, India, Oman, and Kinmen, women had higher prevalence of the metabolic syndrome than men [22]. This finding is not consistent with the study of Mohsin et. al conducted in PIMS, Islamabad. There were 106 patients, which showed a very high frequency of Metabolic Syndrome 91 (85.8%) of whom females (95%) were highly affected. Another factor of female predominance in Metabolic Syndrome is related to the higher frequency of hypertriglyceridemia and low LDH [19].
Hyper-triglyceridemia has been found in 44(64.70%) patients with Metabolic Syndrome where female predominantly affected (59.09%). That finding is also consistent with the finding of the study done in the Diabetes Clinic of Nishtar Medical College and Hospital, Multan was a descriptive cross-sectional study involving a total of 187 Type 2 Diabetic patients that showed 68.4% hypertriglyceridemia with female predominance 42.2% [17]. Mohsin et al. [23] conducted a study in PIMS, Islamabad and among 106 patients, about 78% female showed hyper-triglyceridemia.
In this study the frequency low LDH is 22(32.35%) with female predominance 16(72.73%) where in the study of Mohsin etal conducted a study in PIMS, Islamabad. There were 106 patients which showed low LDH level were present in all female patients [23]. The number of hypertensive patients among the patients with Metabolic Syndrome is 28(41.18%) with a male predominance 16(57.14%) which is also consistent with the study of Mohsin et al. [23] conducted a study in PIMS, Islamabad. There were 106 patients showed 73% male was hypertensive.
The mean age of study population was 58 years ± SD 12.24, ranging from 32-85 years. Majority of the patients in this study were above 40 years (94%). Six (6) cases were found below 40 years. This study showed that 24% patients were in the 4th decade, 25% were in the 5th decade and 29 % were in the 6th decade. Thirty percent of the study population had a positive family history of type 2 diabetes mellitus and 28% of study population had history of tobacco abuse. In individuals with diabetes, the coexistence of other metabolic syndrome factors denotes a higher risk for future development of atherosclerotic cardiovascular disease [24].
The predominant underlying risk factors for the syndrome seem to be abdominal obesity and insulin resistance [25], supported by our study as well. Other associated conditions can be physical inactivity, aging, hormonal imbalance, and an atherogenic diet (e.g., diet rich in saturated fat and cholesterol). The aim of clinical management in individuals with the Metabolic Syndrome was to reduce risk for clinical atherosclerotic cardiovascular disease (ASCVD). Even in people with the Metabolic Syndrome, first-line therapy is directed toward the major risk factors: LDLCholesterol above goal, hypertension, and diabetes [25].
Limitations
i. Single center study with a smaller sample size which may not reflect the exact situation of the disease in the community
ii. A prospective longitudinal study should be done in a large scale on type 2 diabetes mellitus patients and followed up for long time till to develop metabolic syndrome to get more scientific conclusion in this regard
iii. As it was an observational study so explore the frequencies and percentages of Metabolic Syndrome and its relationship between Type II Diabetes Mellitus but confounding variables like hypertension, diabetes mellitus, smoking, dyslipidaemia were not controlled
iv. Logistic regression analysis will be required to get the accurate association and is the major limitation of the study.
Conclusion & Recommendations
A higher frequency of metabolic syndrome (68%) in 100 patients of Type 2 Diabetes Mellitus was found and the frequency of metabolic syndrome is more than double in women (48%) compared to men (20%), central obesity and low HDL were significantly more prevalent in women in compared to men where hypertension was significantly prevalent in men as compared to women. So, it would be reasonable to conclude that women are more likely to suffer from metabolic syndrome that is at the risk of cardiovascular morbidity and mortality. The following measures should take to overcome like weight reduction measures, control blood pressure and dyslipidemia.
To More articles in Current Research in Diabetes & Obesity Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php


Comments
Post a Comment