Psychological Predictors of Weight Loss Success Following Roux-en-Y Gastric Bypass _Juniper Publishers
CURRENT RESEARCH IN DIABETES & OBESITY JOURNAL JUNIPER PUBLISHERS
Authored by
Hazem N Shamseddeen
Abstract
Background: Weight loss is a primary outcome measure for the success of Roux-En-Y gastric bypass (RYGB). Much attention has been paid to the negative effects of psychology on postoperative weight loss. We sought to identify personality traits and eating habits that predict weight loss success following RYGB.
Methods: A single psychologist prospectively evaluated 346 patients, who subsequently underwent laparoscopic RYGB. Psychological evaluation included Minnesota Multiphasic Personality Inventory Short Form (MMPI-2 SF) and long form subscales (MMPI-2 RC) as well as Overeating Questionnaire (OQ). Demographic, anthropomorphic, and clinical data were collected before and after surgery.
Results: The overall mean percent excess weight loss (%EWL) was 71.34+/-24.35%. Of the ten MMPI-2 SF scales, Masculine-Feminine (MF), Hypochondriasis (HS), Schizophrenia (SZ), and Mania (MA) correlated to %EWL, but only MA reached statistical significance (r=-0.24, p<0.005). Of the nine MMPI-2 RC scales, Somatic Complaints (SC), Cynicism (CY), Aberrant Experiences (AE), and Hypomanic Activation (HA) correlated to %EWL, with AE (r=-0.17, p<0.05) and HA (r=-0.15, p<0.005) reaching statistical significance. Of the ten OQ scales, Health Habits (HH), Rationalizations (RA), and Motivation to Lose Weight (MLW) correlated to EWL, with MLW reaching statistical significance (r=-0.59, p<0.005).
Conclusion: This study corroborates the effectiveness of RYGB in achieving weight loss and shows that psychological factors can impact weight loss success. While several personality traits and eating habits correlate with improved weight loss, MA, AE, HA, and MLW seemed to have particularly strong correlations with weight loss success.
Keywords: Morbid obesity; Roux-en-Y gastric bypass; Psychological evaluation; MMPI-2; Overeating questionnaire; Weight loss; Bariatric surgery
Introduction
Obesity has been increasing globally over the last three decades, and its national and global burden has been projected to grow in the future [1,2]. Bariatric surgery is an effective tool for the management of morbid obesity, and several studies have reported decreased mortality and morbidity after bariatric surgery compared to conventional therapy [3,4]. Preoperative psychological screening of bariatric patients is performed at many centers specializing in weight loss surgery, following the consensus statement on bariatric surgery from the National Institutes of Health [5,6]. This statement, however, did not specify the nature of the evaluation, characterize how to utilize the information to determine surgical candidacy, or identify the role such data may play in the postoperative management of patients.
The determinants of obesity are complex and might involve several environmental and psychosocial factors that interact together. Several studies have correlated the psychosocial factors related to obesity and eating habits with surgical outcomes specific to weight loss and weight loss maintenance [7-13]. Other studies focused on the relationships between behavioral traits and postoperative patient compliance and weight regain [14,15]. Preoperative psychological screening is a prominent component of our bariatric surgery program. This screening focuses on identifying psychiatric disorders, characterizing personality traits, and assessing attitudes toward eating. We sought to determine the effects of personality traits and eating habits on weight loss after Roux-en-Y gastric bypass (RYGB).
Materials and Methods
Over five years, a single psychologist prospectively evaluated 605 patients in preparation for bariatric surgery at our institution. Comorbidity and anthropomorphic data were also collected prospectively for clinical purposes. Patient records were then reviewed under approval from the Institutional Review Board for the purposes of this study. The single inclusion criterion for this study was completion of a minimum of10 months of postoperative follow-up.
Psychological evaluation primarily included Minnesota Multiphasic Personality Inventory (MMPI-2) and the Overeating Questionnaire (OQ). Initially, we relied on the long form (MMPI- 2), which consists of 567 questions, and evaluated patients based on the MMPI-2 Restructured Clinical (RC) scales. Over the study period, the algorithm for psychological testing evolved with experience. The MMPI-2 Short Form (MMPI-2 SF) (which consists of the first 370 questions on the MMPI-2) was substituted for MMPI-2 RC to minimize the discomfort expressed by morbidly obese patients during the long period of testing. Additionally, the OQ was not yet available at the beginning of the study period. Once available, we chose to include this questionnaire in an attempt to more fully evaluate bariatric surgery candidates. Thus, the study population contains patients who completed the MMPI- 2 SF only (Group 1, n=114), the entire MMPI-2 only (Group 2, n=44) or the OQ only (Group 3, n=23). The majority of patients completed the entire MMPI-2 and the OQ (Group 4, n=165). Thus, 209 patients completed the entire MMPI-2. Since the MMPI-2 SF simply consists of the first 370 questions of the MMPI-2, MMPI- 2 SF subscales were available for these 209 patients in addition to the 114 patients who completed MMPI-2 SF only, for a total of 323 patients. OQ data were available for the 23 patients who only completed this form and the 165 patients who completed OQ in addition to MMPI-2. Ultimately, MMPI-2 RC data were available for 209 patients, MMPI-2 SF data were available for 323 patients, and OQ data were available for 188 patients.
Weight loss data were collected during clinical encounters with the bariatric surgery program preoperatively and at each postoperative appointment. All patients in this study underwent laparoscopic Roux-en-Y gastric bypass (LRYGB). No other primary bariatric procedures were performed at our program during the study period. All data are presented as mean+/- standard deviation. Data were analyzed using ANOVA for multiple comparisons of means of continuous variables and Fisher's exact test for comparisons of discrete variables. Pearson and Spearman coefficients were calculated to examine correlations between questionnaire variables and postoperative excess weight loss. Statistical significance was set at alpha=0.05 for all analyses.
Results
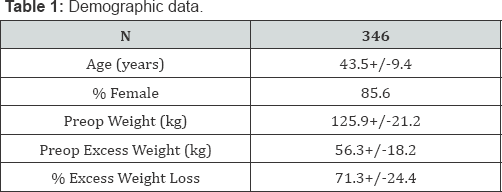
Over a five-year period, 605 candidates for bariatric surgery underwent pre-surgical psychological testing by a single psychologist. At the time of data analysis, 346 patients had undergone RYGB and achieved postoperative follow-up between 10 to 24 months. The remaining patients had not undergone surgery (n=114) or had not reached the minimum follow-up of 10 months (n=145). Of the patients who had not reached 10 months of follow-up, 57 patients did not return to clinic and, thus, werelost to follow-up. The study population consisted of 346 patients with a mean age of 43.5+/-9.4 years (Table 1). The patients were primarily females (85.6%). Mean preoperative weight was 125.9+/-21.2 kg, and mean preoperative excess weight was 56.3+18.2 kg. On average, patients were able to achieve 71.3+/-24.4% excess weight loss. Preoperative psychological evaluation was accomplished via MMPI-2 SF (n=323), MMPI-2 RC (n=209), and OQ (n=188), with 165 patients completing all three instruments. There were no significant differences in demographic data among the patient groups (1-4 as described in methods section) in terms of age, gender proportions, preoperative excess weight, or postoperative excess weight loss.
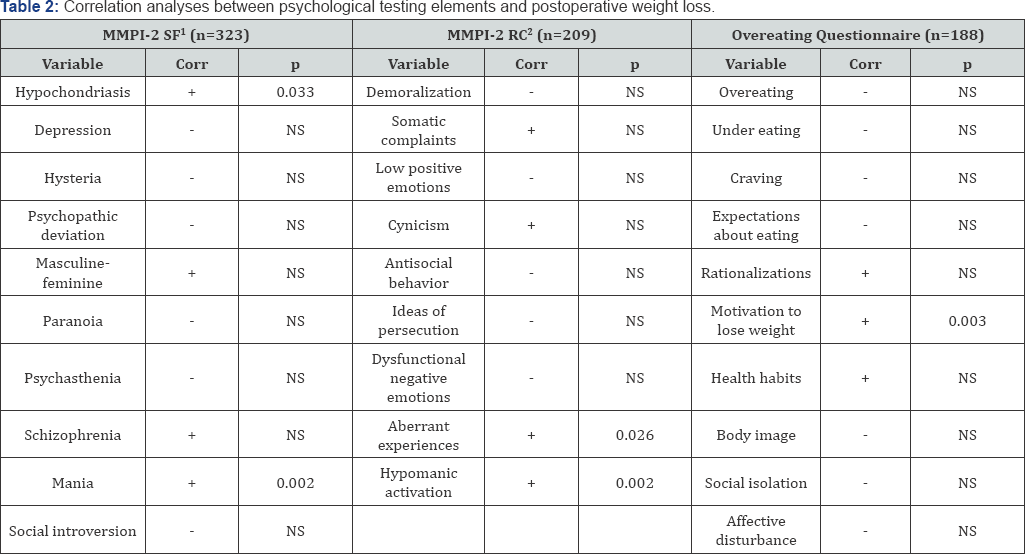
Correlation analyses between MMPI-2 SF, MMPI-2 RC, and OQ subscales and the percentage of excess weight loss (%EWL) following RYGB are summarized in Table 2. Only four of the ten subscales of the MMPI-2 SF correlated with greater postoperative %EWL. The masculine-feminine (r=-0.10, p=0.07) and schizophrenia (r=-0.10, p=0.07) subscales showed a correlation with %EWL but did not reach statistical significance. Hypochondriasis (r=-0.12, p=0.03) and mania (r=-0.25, p<0.0001), on the other hand, significantly correlated with greater %EWL following LRYGB. The remaining subscales (depression, hysteria, psychopathic deviation, paranoia, psychasthenia, and social introversion) did not correlate with %EWL. Similarly, four of the nine MMPI-2 RC subscales exhibited a correlation with %EWL. Somatic complaints (r=-0.13, p=0.06) and cynicism (r=- 0.12, p=0.08) demonstrated correlations with %EWL that were not significant. Statistically significant correlations with %EWL were identified for hypomanic activation (r=-0.16, p=0.02) and aberrant experiences (r=-0.21, p=0.002). The remaining subscales (demoralization, low positive emotions, antisocial behavior, ideas of persecution, and dysfunctional negative emotions) did not correlate with %EWL. As for OQ, the rationalizations (r=- 0.12, p=1.0) and health habits (r=-0.14, p=0.06) exhibited nonsignificant correlations. The motivation to lose weight subscale, however, correlated strongly with %EWL, as evidenced by r=- 0.59. This correlation was statistically significant (p<0.0001). The remaining OQ subscales (overeating, undereating, craving, expectations about eating, body image, social isolation, and affective disturbance) did not demonstrate a relationship with %EWL.
Discussion
Morbid obesity is a multifactorial disease which has been growing at an alarming rate [16]. The current epidemic nature of morbid obesity has motivated a great deal of research aimed at elucidating its causes. It has become clear that the predisposition to obesity begins with genetic tendencies [17]. The resulting metabolic dysregulation disrupts energy homeostasis and leads to the accumulation of adipose tissue [18]. The adipose tissue, in turn, perpetuates the metabolic abnormalities through significant endocrine activity which affects many organ systems [19,20].
Yet, there are documented psychosocial and environmental facets to this disease [21]. It is unclear whether this is simply the result of individual and societal behaviors or the result of interaction of the brain within the disordered metabolic milieu. Regardless of the cause, the impact of behavior and personality on the development of obesity are undeniable. Psychological screening is considered an important component ofcomprehensive care of the bariatric surgery patient [5,6]. While several studies have discussed the psychological profiles of bariatric surgery patients, there is little consensus as to the elements that should be considered when evaluating patients [22,23]. While no current instrument can reliably predict patient weight loss outcomes, there is evidence that eating behaviors and personality traits can be useful in assessing bariatric surgery candidates [22,24].
The MMPI-2 questionnaire is widely-used to evaluate psychosomatic conditions and to identify personality traits [25,26]. This instrument is valid for assessing obese patients [27]. Some investigations have demonstrated that obese patients have an increased prevalence of psychopathology on MMPI-2 [27], while other work did not find a correlation between psychopathology level and obesity [28]. The OQ is an 80-item instrument that measures attitudes toward obesity and eating. The OQ provides scores in ten areas. Six areas reflect general health habits and assess psychosocial functioning. The other four areas target psychosocial issues that coexist with obesity. The OQ is reputed to assist in planing effective weight loss efforts for patients. In our study, personality characteristics and attitudes toward eating correlated with %EWL at 12 to 24 months following LRYGB. Between the RC subscales and the SF subscales, eight elements of MMPI-2 correlated with better %EWL, as indicated by r <-0.1, with four of these elements (hypochondriasis, mania, aberrant experiences, and hypomanic activation) reaching statistical significance (Table 2). Three subscales of the OQ correlated with improved %EWL, but only one (motivation to lose weight) was statistically significant (Table 2).
Other investigators have used MMPI-2 to evaluate patients in preparation for RYGB [13,29]. One such study identified that some scales were associated with better weight loss outcomes at six months post surgery [13]. Furthermore, some scales were associated with weight loss at various postoperative intervals, such that the investigators suggested a potential role for time- dependent postoperative patient management strategies [13]. Another study identified an "emotionally disturbed" patient group, based on the MMPI-2, and found that these patients were less compliant and had decreased weight loss [29].
In terms of evaluating attitudes toward eating, Powers et al studied eating pathology in bariatric surgery patients preoperatively and found no relationship between presurgical eating pathology and weight loss [30]. Yet, in a review of the literature, Niego et al found that patients with preoperative binge eating behavior were more likely to continue the eating pathology following surgery and achieve less weight loss [31]. These assertions are supported by Kalarchian et al, who found that the recurrence of binge eating after surgery was associated with weight regain [9]. Finally, it has been reported that risk for weight regain following bariatric surgery can be predicted during preoperative screening, as primarily indicated by increased food urges, decrease well-being, and concerns over addictive behaviors [14].
Our study differs from a large portion of the available literature in that we focused on identifying predictors of weight loss success rather than weight loss failure. We were able to identify correlations between improved weight loss and certain psychological traits and eating habits. In our practice, we plan to combine our findings with the available literature to preoperatively identify traits that may motivate a patient to succeed as well as those that may predispose to failure. The ultimate goal is to address the predictors of failure while promoting the predictors of success in an attempt to maximize the benefits of bariatric surgery to the patient. Psychological screening will continue to be part of preoperative screening for bariatric surgery in many programs. We were able to identify personality and eating-associated traits that correlated to weight loss success followingLRYGB. Further investigation is warranted in this field to more fully understand how to support patients along the weight loss journey and maximize postoperative weight loss and weight loss maintenance.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php


Comments
Post a Comment