Waist to Height Ratio is the Preferred Way to Measure the Association between Obesity and Bisphenol a Exposure
CURRENT RESEARCH IN DIABETES & OBESITY JOURNAL JUNIPER PUBLISHERS
Authored by Nathaniel R Geyer
Abstract
Bisphenol A-induced weight gain using four body measurements (body mass index, waist circumference, waist to height ratio & adult body fat percentage), in adults 18-74 years has been connected with obesity and diabetes. So a cross-sectional analysis of urinary bisphenol A concentrations by four body measurements, using six pooled datasets from the 2003-2014 biennial National Health and Nutritional Examination Surveys. After adjustment by survey year, age, race, gender, diabetic status, education level, and smoking status, obesity was positively associated odds ratios of having bisphenol A exposure in each of the four body measurements. In addition, bisphenol A exposures of 1.73-3.52ng/mL had highest chances of being either obese or overweight. Higher bisphenol A exposure had association with obesity when using the waist to height ratio cutoff (≥0.58) as compared with the three other measures that can be calculated with the biennial dataset. This correlation suggests that waist to height ratio should be preferred over the other three body measurements examined.
Keywords: BPA; NHANES; Obesity; WHtR
Abbreviations: BPA: Bisphenol A; NHANES: National Health and Nutrition Examination Survey; BMI: Body Mass Index; WHtR: Waist to Height Ratio; WC: Waist Circumference; ABF%: Adult Body Fat Percent; WHR: Waist to Hip Ratio
Introduction
In the United States there has been a chronic epidemic of people who are obese or overweight, which has a connection with diabetes and other disorders. However, the definition of obesity has been highly connected with BMI, which is basically a height to weight ratio. There have been calls in research to try other definitions of obesity using WC, WHtR, and ABF%. The challenge is that these are not as well-known and cut-off points are not as understood.
Obesity measurements
As compared to BMI and WC, WHtR has a higher threshold for detecting cardio-metabolic factors (hypertension, obesity, type-2 diabetes, dyslipidemia, metabolic syndrome & other cardiovascular outcomes) those other two measures, using a sample of more than 300,000 adults in several ethnic groups, ages, and genders, suggesting that WHtR be an important screening tool [1]. Higher waist to height ratio (≥0.50) was found to have 35% of people with no increased risk using BMI or waist circumference to have significantly higher cardio-metabolic risk factors [2]. In addition, a sensitivity analysis found that WHtR represents the best predictor of cardiovascular risk followed by WC and WHR, and discourages the use of BMI [3] or related formulas for ABF% [4]. A Chinese study found that the international cutoff (≥0.50) corresponded with overweight and approximately 0.58 with obesity [5]. In a previous study from NHANES found that a WHtR cutoff of 0.580 is optimal for cardio-metabolic factors, which is an improvement over the 0.50 international cut off, in adults [6].
BMI was calculated in NHANES as weight (kg) divided by height (m2), using the <25, 25-30, and ≥30kg/m2 cut off points. Body Elevated waist circumference was measured using the national cholesterol education program expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) criteria as ≥102cm in men and ≥88cm in women. In addition, WHtR was calculated as [WC/Height] and ABF% as [(1.20 x BMI)+(0.23 x Age)-(10.8 x Gender) -5.4] from these two equations [1,4]. Consistent with literature the cutoffs for WHtR were 0.50-0.58 for overweight and ≥0.58 for obesity [5]. The ABF% from BMI included males (<20, 20-30, and ≥30) and females (<32, 32-40, and ≥40) [4]. WHR cannot be estimated in NHANES because hip circumference was not measured.
Bisphenol A and obesity
Previous studies have supported a link between low dose exposure to endocrine disrupting chemical and obesity such as BPA, which are commonly found in plastics, dental equipment, food, and beverage cans [7,8]. However, with four possible body measurements in NHANES makes it a challenge to clearly identify the association with BPA and obesity. An older study by car wile and michels found an association with obesity and urinary BPA using an older cross-section of NHANES, using just BMI and waist circumference [7]. Using urinary BPA exposure in a large pooled biennial cross-sectional study NHANES makes it possible to identify the measure that best predicts obesity.
Conclusion
In the subset of 9,449 adult participants surveyed in the pooled 2003-2014 NHANES data set the geometric mean creatinine adjusted urinary BPA concentration was 1.78μg/g, which was lower than a previous finding [7]. However, when doing correlations matrices of the confounders it was found that creatinine was correlated with urinary BPA concentration (Spearman’s correlation=0.58) so the variable was excluded as a potential confounder, in the logistic regression models. It was observed the BPA concentration was highest in men, younger people, smokers, diabetics, and racial-ethnic minorities. After adjustment, using multinomial logistic regression modeling, by survey year, age, race, gender, diabetic status, education level, and smoking status people with a BMI greater than 30 were associated with higher BPA levels, with odds ratios ranging from 1.66 to 2.10 (Table 1). This association was also observed in the overweight individuals but with lower odds ratios. People having excessive WC or abdominally obese were also more likely to have higher BPA levels, after adjustment by the same variables ranging from 1.30-1.57. People with higher WHtR were also more likely to have higher BPA levels. However, in the overweight group (0.50-0.58) it was inversely associated with BPA, suggesting that a low dose of BPA has the biggest effect on WHtR. The highest association was with ABF% which uses BMI plus age and gender to make a calculation. This calculation resulted in odds ratios ranged from 1.53-2.53, suggesting an increased chance of being connected with a high urinary BPA levels. However, unlike WHtR measurement, there was also no significant association with being overweight except in people classified in quartile 3(1.73-3.52ng/mL), for ABF%.
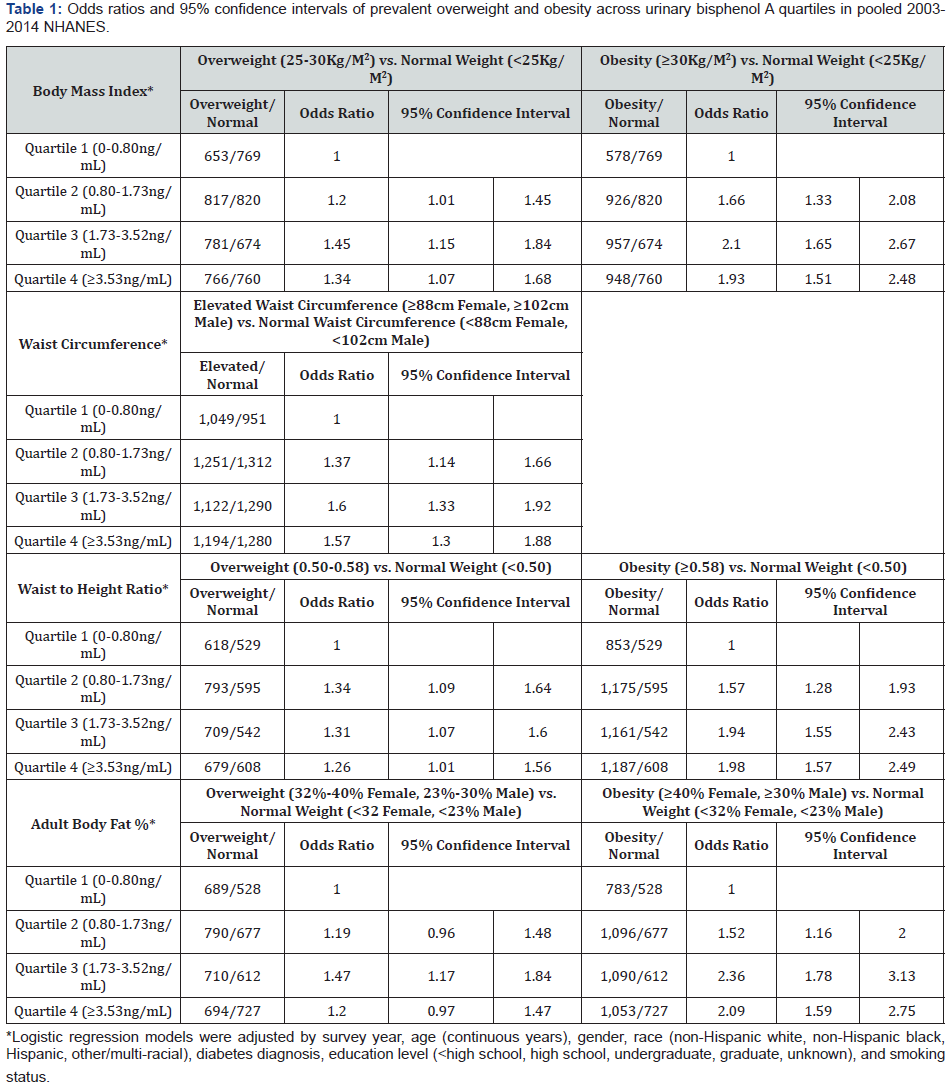
In this cross-sectional analysis of pooled 2003-2014 NHANES data high urinary BPA levels were associated with obesity as defined using the four body measurements. This analysis takes into consideration a large biennial dataset with fairly consistent measures of environmental exposures such as urinary BPA levels. Out of all of the four measurements there was a clear association that increased BPA exposure is associated with obesity. The difference in the four measurements with large sample size was small but it clearly shows that with additional information as found with % adult body fat with BMI characteristics had the lowest sample size (n=2,272) for obesity, but had the highest association with an elevated BPA exposure. By comparison, higher waist circumference (n=4,833), BMI (n=3,023), and adult body weight percentage (n=2,544) were not as associated with high urinary BPA exposures. Higher BPA exposure had the highest association with obesity when using the waist to height ratio cutoff (≥0.58) as compared with the three other measures that can be calculated with this dataset. This correlation suggests that WHtR should be preferred over the other three body measurements examined.
To More articles in Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php


Comments
Post a Comment