Analysis of Inflammatory Cytokines in Pre-Diabetic Subjects
Authored by Saket Gupta
Abstract
Objective: Pre-diabetes is defined as either impaired fasting glucose ((IFG) between 5.6 and 6.9mmol/l) or impaired glucose tolerance (IGT) wherein fasting or post-prandial plasma glucose levels are above normal levels, but below that of clinical Type-2-Diabetes Mellitus (T2DM). Both IFG and IGT, risk factors for T2DM and macrovascular diseases, have previously been linked with inflammation. With this in mind, we sought to comparatively evaluate the levels of inflammatory markers in pre-diabetics relative to normal healthy individuals.
Methods: We determined the levels of serum cytokines in a cohort of 9 patients with pre-diabetes and thirty four individuals with normal glucose control using a 96-Well Multi-array 7-plex assay or 1-plex IFN-β and Rantes 96-well plates (Meso Scale Discovery, Gaithersburg, Maryland, USA).
Results: Our study demonstrated that the patient group with pre-diabetes exhibited a non-significant trend towards elevated IL-6, TNFα, IFN-β, IL-12, Rantes, IL-10 and IL-8 when compared with the healthy controls group. After adjustment for age, sex, BMI and WHR, in the study population, there was no difference in the levels of cytokines between the pre-diabetes and normal groups.
Conclusion: Measurement of serum cytokine levels alone is unlikely to be a predictor of clinical disease activity in individuals with pre-diabetes.
Keywords: Pre-diabetes; Inflammation; Pro-inflammatory cytokine
Introduction
Pre-diabetes may be defined as either an impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) wherein fasting or post-prandial plasma glucose levels are above normal levels, but below that of clinical Type-2-Diabetes Mellitus (T2DM) [1]. Elevated haemoglobin A1c, or glycosylated haemoglobin (HbA1c) of 5.7% to 6.4%, as per American Diabetes Association is also denoted as an indicator of pre-diabetes [2]. Together with obesity, both IFG and IGT are risk factors for T2DM and macrovascular diseases. Given this, it is arguable whether screening for pre-diabetes should be undertaken on the premise that the health benefits outweigh the cost implications.
Studies have reported that inflammatory cytokines (IL-1β, IL-6) and C-reactive protein are elevated in patients with T2DM [3,4]. Following on from this, several studies have investigated and reported that pro-inflammatory cytokines are elevated in patients with IGT [5,6] and predicted the progression to T2DM [4]. However, there is paucity of data exploring whether perturbations occur in the level of other cytokines, such as IL-12 and IFN-β and chemokines in the context of pre-diabetes. With this in mind, we analysed a cohort of 43 healthy Irish subjects to evaluate the relationship between pre-diabetes and circulating cytokine levels.
Materials and Methods
Study subjects and design
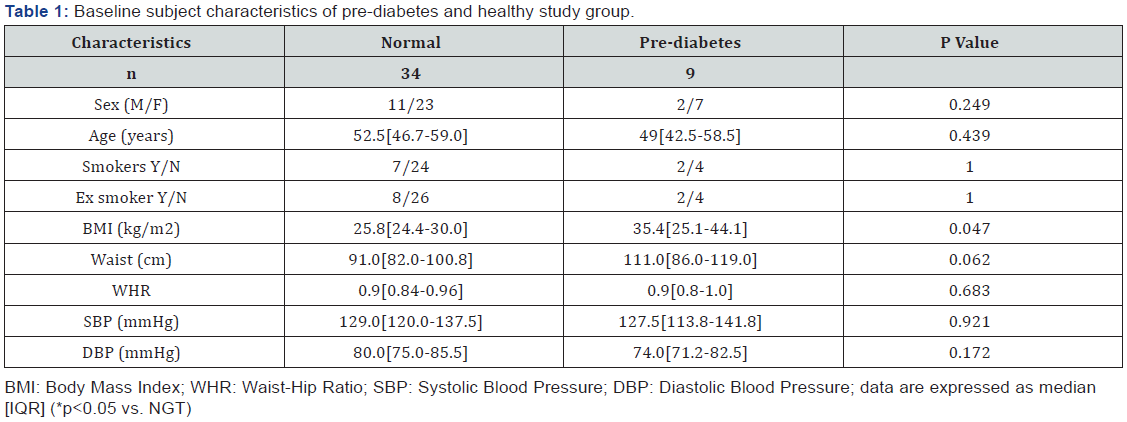
Thirty four healthy control participants with normal glucose control (NGT) were recruited to the study, as described in our previous study [7]. The healthy control participants were screened for diabetes using the standard oral glucose tolerance test (American Diabetes Association (ADA)) and individuals with abnormal blood results (diabetes or pre-diabetes) and individuals with a history of chronic illness and/or individuals taking medication were excluded from the NGT group. Nine prediabetes participants were recruited to the study. Of the nine pre-diabetes subjects, eight subjects had IFG and one subject had IGT (Table 1) and were diagnosed as having pre-diabetes based on the ADA criteria following an OGTT test (Table 2 [8]). Participants with pre-diabetes were healthy volunteers and were not on any medications. All participants were >18 years old and were not pregnant. Exclusion criteria included the following: Evidence of current infection (white cell count >11 or significantly elevated CRP), current treatment with antibiotics, neutropenia (a leucocyte count of less than 2000 per cubic millimetre), pregnancy or breast-feeding, non diabetic renal disease or liver disease (a level of asparate aminotransferase or alanine aminotransferase of more than three times the upper limit of the normal range), ongoing or previous cancer and the use of oral/inhaled glucocorticoids, immunosuppressive treatment or immunodeficiency. Participants with abnormal results were excluded from the study. Personal and medical data were obtained by patient interview, by using hospital medical notes, and from using hospital blood test results. The demographic information was obtained from research participants and their weight, height, blood pressure & waist and hip circumferences were determined. BMI was calculated as body weight (in kilograms) divided by body height (in meters) squared. Waist-to-hip ratio (WHR) was calculated as waist divided by hip circumference. Informed consent was obtained from all participants and the protocol was approved by the Midlands Research Ethics Committee, Health Service Executive, Ireland, and by the Ethical Review Board, Maynooth University, Maynooth, Ireland.
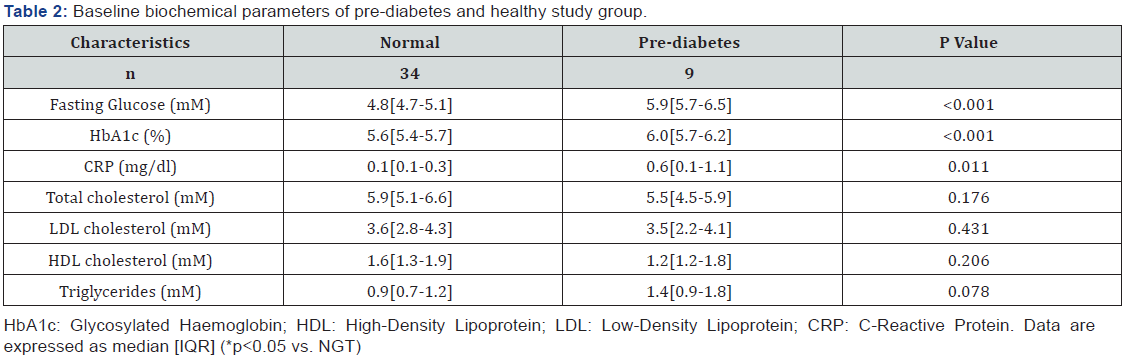
Biochemical analysis
Following the collection of 40ml of peripheral blood from consenting fasting study participants between 8 and 10am (to minimise the impact of diurnal variation), various biochemical parameters and cytokines were measured. HbA1C was measured using a haemoglobin analyser HA-8160 (Menarini Pharmaceuticals, Ireland). Whole blood counts were measured using an Advia analyser. Lipid profile, urea, creatinine, sodium, potassium, asparate aminotransferase, alanine aminotransferase, bilirubin, alkaline phosphatase, gamma glutamyl transferase, CRP, ferritin, coagulation screen, thyroid profile and plasma glucose levels were measured using a Roche Modular 1800 analyser. An early morning urine sample was also collected for the measurement of ACR.
Cytokine measurements
For cytokine analysis, the blood sample was placed on ice and then centrifuged at 3000rpm for 5min at 4 oC within 1 hour of venesection. Serum was collected and stored at -80 °C until required. Levels of serum TNFα, IL-6, IL-1β, IL-10, IL-8, IL-12p70 and IFN-γ were determined using a 96-Well Multiarray 7-Multiplex Assay (Meso Scale Discovery, Gaithersburg, Maryland 20877, USA). Levels of serum IFN-β and Rantes were determined using single-plex 96-well plates (Meso Scale Discovery, Gaithersburg, Maryland, USA).
Statistical analysis
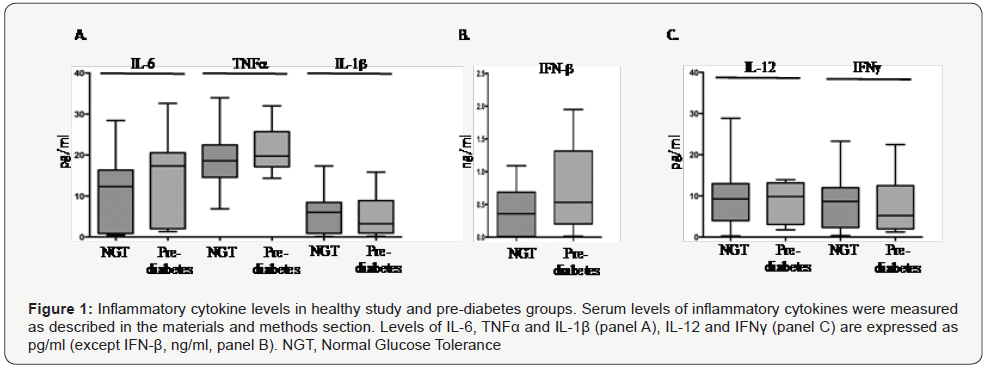
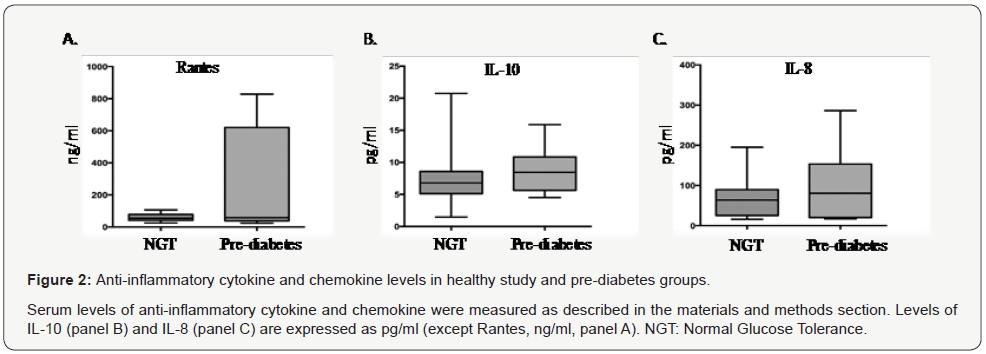
Data are expressed as median (interquartile range) and represented as box-and-whiskers plots wherein the dark midline in the box represents the distribution’s median value. The top and bottom edges of the box respectively represent the 75th and 25th percentile values. The top and bottom of the vertical lines, the whisker respectively represent the upper and lower maximum value. χ2 test or Fisher exact test (as appropriate) were used to compare proportions. The Mann-Whitney test was used in case of non-normally distributed parameters to compare median between two groups. Data were transformed to log normal format and multifactorial ANOVA was applied to evaluate the effect of variables (age, sex, BMI, WHR and duration of diabetes) on different inflammatory markers. Correlations between values were examined by calculating Spearman correlation coefficients. All the statistical analysis was performed using the Prism 6.0 computer program (GraphPad, La Jolla, CA) and p values less than 0.05 were considered significant.
Results
Participant characteristics
The median age and smoking status was comparable in the pre-diabetes and the normal glucose control study groups. In the NGT group, 20.5% were smokers and 30.7% were ex-smoker, whereas in the pre-diabetes group, 22% were smokers and 28.6% were ex-smoker (Table 1). The pre-diabetes study group exhibited a significantly higher BMI when compared to the NGT control group (p<0.05). However, no significant difference was seen in the WHR and blood pressure between the two groups. The fasting glucose and HbA1c was significantly higher in the prediabetes study group when compared to the NGT study control group (p<0.05). Interestingly, levels of CRP were significantly elevated in the pre-diabetes study group when compared to the NGT study group (p<0.05). However, no significant differences in the lipid profile were observed between the two groups (Table 2).
Analysis of cytokine levels in patients with NGT and IGT
Our data shows a trend towards elevated serum levels of IL- 6, TNFα and IFN-β in the pre-diabetic study study group when compared with healthy control group (Table 3); however, the differences were not statistically significant (Figure 1A & 1B). Further, serum levels of IL-12 were marginally higher in the prediabetic patient group when compared with the normal glucose control study group (Table 3 and Figure 1C). In contrast, a trend towards lower levels of IFN-γ among the pre-diabetic study group when compared with the healthy control group was seen (Figure 1C). Levels of Rantes were marginally higher in the prediabetic study group when compared to the group with normal glucose control (Figure 2A and Table 3). Similarly, serum levels of the chemokines IL-10 and IL-8 were marginally higher in the pre-diabetes participant group when compared with healthy control group (Figure 2B & 2C). Notably, the differences in cytokine levels did not reach statistical significance.
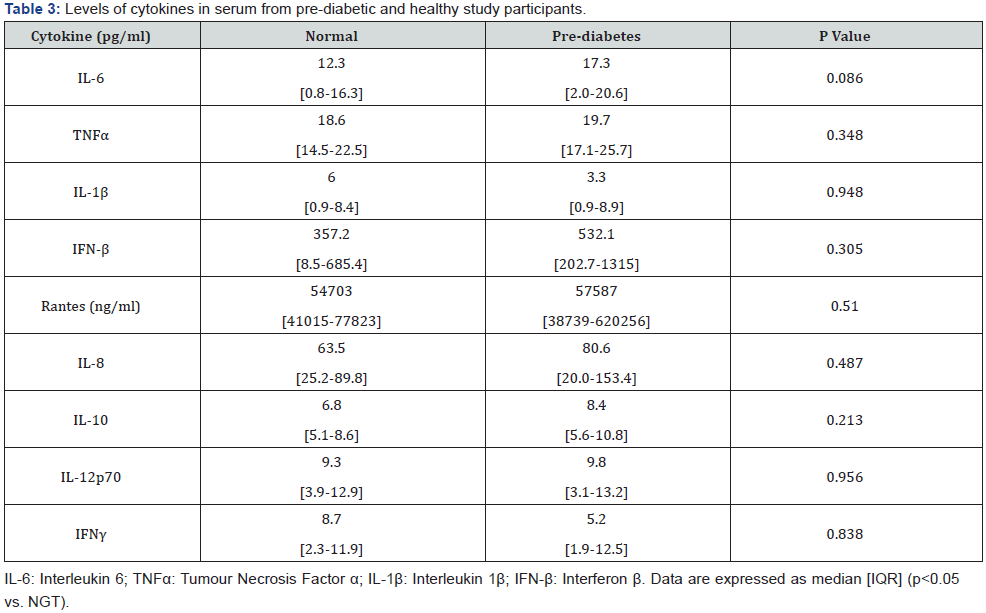
Following multifactorial ANOVA, applied on all cytokines measurements using lognormal values and adjustment for age, sex, BMI and WHR, it was found that there were no significant differences in cytokine levels between the pre-diabetes study group and the group of individuals with normal glucose control.
Discussion
Herein, we sought to establish whether perturbations in inflammatory markers were evident among individuals with pre-diabetes and whether measurement of serum cytokine levels alone may be a predictor of clinical disease activity in individuals with pre-diabetes. To do this, thirty four healthy control participants were recruited to the study and are further described in another study that we undertook [7]. Concurrently, nine pre-diabetes participants were recruited to the study and are described herein. While the prevalence of pre-diabetes is approximately 30% in the general population (UK/USA) [9,10], it was noted that the aforementioned group were generally not captured as a study population presenting to the Endocrinology clinic, Midlands Regional Hospital, Mullingar. Therefore, in terms of the recruitment of pre-diabetes study participants at this location, while eight of the individuals were identified during the course of our efforts to recruit healthy individuals, as described in our previous study [7], one individual was identified following a GP referral. Despite our best efforts and in the context of our strict inclusion/exclusion criteria and ethical approval, it was only possible to recruit a total of nine pre-diabetes individuals to the current study. Notably, treatment-naïve pre-diabetes subjects were required for the study and therefore limited the number of individuals that could be recruited to the pre-diabetes study group. Following recruitment of the study participants, we comparatively assessed the inflammatory milieu of pre-diabetes study participants and healthy individuals. The BMI of the prediabetic study group was significantly higher than that of the healthy control group, as was the fasting glucose and HbA1c levels of the pre-diabetic group. In contrast, the lipid profile of the pre-diabetic study group was comparable to that of the healthy control group.
Regarding the pro-inflammatory cytokine levels, we found that the pre-diabetes study group tended to have elevated levels of the pro-inflammatory cytokines, IL-6, TNFα and IFN-β, when compared with the normal glucose control group. Further, while IL-12 levels was slightly higher in the pre-diabetes study group, IFN-γ levels were lower in the pre-diabetic group when compared to individuals with normal glucose control. In addition, there was a trend towards elevated levels of Rantes, IL-10 and IL-8 in the group with pre-diabetes when compared with the healthy control group. Notably, the differences in cytokine levels among the groups failed to reach statistical significance. Further, after adjustment for age, sex, BMI and WHR, there were no differences in the levels of cytokines between the pre-diabetic and normal study groups
Our findings are in contrast to that previously reported by Spranger et al. [3] who showed that levels of plasma IL-6 and TNFα, but not IL-1β, were associated with future T2DM. Furthermore, the study reported that following adjustment for age, sex, BMI, alcohol consumption, waist-to-hip ratio (WHR), smoking status and HbA1c, IL-6, but not TNFα or IL-1β, was identified as an independent predictor for T2DM [3]. Another study reported an association between elevated levels of IL-6 and CRP and the risk of developing T2DM in the future and the link remained significant following adjustment for BMI, family history of diabetes, smoking, exercise and alcohol use using multivariate analysis [4]. More recently, studies have shown that HbA1c and IL-6 levels were significantly higher in IFG and IGT patients when compared to healthy individuals [11,12].
Conclusion
In summary, our data suggests that the pre-diabetic patient group do not exhibit statistical significant differences in circulating cytokine levels when compared to the normal healthy group. Further, it is noted that multiva
riate analysis confirmed that there were no significant differences following adjustment for age, sex, BMI and WHR. However, though non-significant, it is noted that our study showed a trend towards elevated levels of serum IL-6, TNFα, IFN-β and IL-8 among the pre-diabetes group. It is plausible to speculate that the robustness of our study would be enhanced by the recruitment and inclusion of additional study participants to the pre-diabetes group. However, as previously indicated, the inclusion of additional pre-diabetes participants was beyond the scope of the current research due to the confined nature of our study criteria.
Importantly, our study shows that the measurement of serum cytokine levels alone in individuals with pre-diabetes may not serve as a robust readout of pre-diabetes state. In conclusion, our study shows that our pre-diabetic group present with a nonsignificant trend towards elevated levels of serum cytokines that may be linked with confounding factors such as BMI, WHR, age and gender. Based on these results, serum cytokine levels alone is unlikely to be a predictor of clinical disease in individuals with pre-diabetes.
To More articles in Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php



Comments
Post a Comment