Gastric Emptying after Sleeve Gastrectomy for Morbid Obesity: Current Knowledge andInferences on GORD_Juniper Publishers
CURRENT RESEARCH IN DIABETES & OBESITY JOURNAL JUNIPER PUBLISHERS
Authored by Mohamed Bekheit
Abstract
Laparoscopic sleeve gastrectomy is a relatively quick and straightforward procedure that offers high weight loss with few complications. Amongst the bariatric procedures, however, it has been reported that LSG has a higher incidence of gastroesophageal reflux which leads to poorer quality of life and increased risk of gastro-esophageal cancers. The proposed mechanisms behind this are many including modification of the oesophageal sphincter, increased gastric pressure gradients and changes to gastric anatomy.
It appears that sleeve gastrectomies have the effect of modifying the gastric emptying time which is a potential risk factor that could affect the incidence and severity of reflux disease. A faster gastric emptying time would lead to less of a pressure gradient and also less time for gastric contents to reflux. Gastric emptying after a sleeve gastrectomy appears to be faster, and this is because of the way a resection interferes with the regulatory mechanisms behind food. Furthermore, the previously conservative gastrectomies that kept more of the antrum have slower emptying times than more radical antral resections.
We have concluded from the literature that more antral resections would lead to faster gastric emptying times and therefore minimize the risk of GORD in these patients. Much of this literature is recent, however, and a more formal systematic review is needed especially with earlier conflicting studies. Further research is also needed to see whether antral resections can help minimize gastric reflux in the long-term as well as maintain weight loss.
Keywords: Laparoscopic; Sleeve; Obesity; Bariatric; GORD; Emptying
Abbreviations: LSG: Laparoscopic Sleeve Gastrectomy; GORD: Gastroesophageal Reflux Disease; LRYGB: Laparoscopic Roux-En-Y Gastric Bypass
Introduction
Laparoscopic sleeve gastrectomy (LSG) is becoming an increasingly popular choice amongst bariatric surgeons, for the treatment of obesity and its related complications [1], as these are becoming more and more prevalent in the developed world and bariatric surgery is often the only option for their long-term resolution [2]. LSG offers a significant potential weight loss to the patient, while also being a relatively simple procedure compared to the diversional techniques, leading to fewer complications and less severe nutritional deficits [3]. LSG has come under greater scrutiny recently, with regards to its effects on gastroesophageal function [4]. Especially in the context of a growing body of evidence suggesting that patients might develop 'de novo' GORD [5] , as well as exacerbations of previous reflux symptoms [5]. This is relevant as evidence has shown that GORD and obesity both increase a patient's risk of adenocarcinoma of the cardia [6] Links between gastric emptying and GORD, in the context of LSG, have been hinted at in the literature, but, to our knowledge, these have not been reviewed specifically. In this mini-review we aim to establish 1) the effects of LSG on gastric emptying and 2) what effect, if any, this has on GORD. From this, we may be able to form new conclusions on how to modify the procedure to improve patient outcomes.
Gastric emptying after sleeve gastrectomy
Gastric emptying has been studied in obese patients. A review by Xing and Chen 2004 concluded that gastric emptying was unchanged for liquids and accelerated for solids in Obese patients [7,8]. The authors suggested the mechanism was via a reduction of the negative feedback satiety signal, produced by the presence of food in the stomach, precipitating a feeling of hunger and shortening the interval between consecutive meals. This would make sense, as delayed gastric emptying would be associated with upper GI symptoms (early satiety, nausea, and vomiting, etc.) and reduced food intake, as frequently seen in patients with gastroparesis who are frequently underweight [7].
Early studies by Melissas et al. [9,10] showed acceleration of the gastric emptying of solids when tested using scintigraphy [9,10]. These studies showed a decreased of the lag-phase (i.e., time from the end of the meal to the beginning of the emptying into the duodenum). An accelerated T1/2 (time from completion of the meal to the point at which half of the meal left the stomach), and an increased percentage of gastric emptying (the portion of the meal that left the stomach at the end of the observation period of 90 minutes) were also reported. Moreover, they showed that these findings persisted after 24 months [10]. These studies were limited, in that they had small sample sizes (11 and 14; respectively) and were unable to get detailed anatomy using scintigraphic imaging. These early studies were contested by Bernstine et al. [11] (Table 1) concluded that gastric emptying was not affected by sleeve gastrectomy [11].
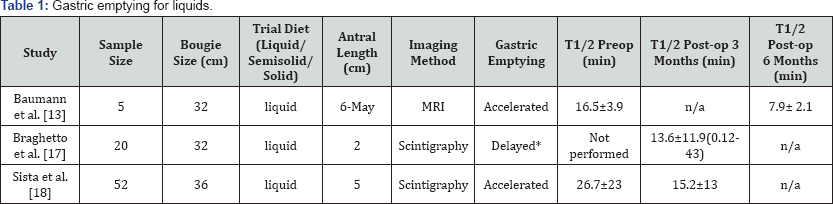
*No preoperative control
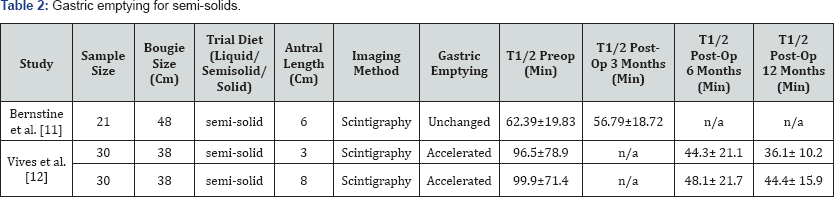
A more recent study by Vives et al. [12] echoed many of the findings by Melissas in that the T1/2 (Table 2) was shorter post LSG but the effect is even greater with a more radical antral resection [12]. This study also adds the CT gastric volume analysis that showed that initial differences in gastric volume between distal and proximal repairs settled after time which would imply gastric physiology has a major role, over gastric anatomy, in the etiology of reflux. As a result of these discrepancies, most authors had recommended further study of the underlying mechanisms involved in gastric emptying. This was carried out by Baumann et al. 2010 who used time-resolved MRI pre- and post-LSG showing that the qualitative pattern of antral motility was preserved even early after surgery, but the proximal part of the stomach, which was now the sleeve, remained almost entirely still without any coordinate peristalsis. They concluded that the stomach after LSG seemed to be divided into two functionally distinct segments: a largely immobile sleeve and an accelerated antrum [13]. They were limited in the small sample size (only 5 patients) and used liquid meals only.
One study attempted to look at voiding time, but used gastrograffin and arbitrarily differentiated 'fast' and 'slow' voiding depending on whether sleeve voiding took more or less than a minute. This study was limited in that it did not use scintigraphy, did not calculate T1/2 and started the resection line at various distances from the pylorus (4cm-6cm), meaning the results have to be taken with caution and are difficult to compare with those from other studies. Having said this, they showed that sleeve voiding was fast in 85.96% of patients and slow in only 14.03% [14].
This hypothesis that the antrum was the locus for accelerated gastric emptying has often led surgeons to leave 7cm of antrum intact when carrying out LSG. The problem with this was that it limited the restrictive ability of the sleeve and theoretically would reduce the intended weight loss long term. As a result, Michalsky et al. 2013 intermittently performed radical pyloric antrum resections, leaving only 2.5cm. Despite a limited sample size (n=4), they found that T1/2 was lower even post- radical antral resection [15]. However, these findings were disputed by Fallatah et al. 2013, who found that when resecting at 4cm from the pylorus 73% showed delayed gastric emptying, compared to when resecting at 7cm from the pylorus 87% of patients showing acceleration [16]. However, this particular study and similar studies [17,18] did not perform a control study before the LSG and therefore, conclusions whether or not LSG caused the delayed gastric emptying are not robust.
A more recent study concurred with Michalsky with a larger sample size (n=60) and this also suggested that the more radical antral resection correlated with a faster gastric emptying time [12]. LSG can affect gastric emptying via a number of different mechanisms, including altered contractility, altered gastric distensibility, and resection of the gastric pacemaker situated at the large curvature [12,19]. Initially, concerns were raised about the risks of resecting the fundus, where the gastric pacemaker is thought to be located, as this might delay emptying. However, as highlighted by [13], gastric motility is not controlled by a single anatomically localized pacemaker, but instead a network of interstitial cells of Cajal (ICC) in the myenteric plexus, responsible for slow waves leading to smooth muscle contraction [13]. One of the reasons why even after resection of the greater curvature, gastric emptying is preserved was suggested in a study, which showed that these slow waves could be generated in isolation in the antrum [20]. The concern then, was that too radical a resection would delay gastric emptying. However, [12] suggested the opposite might be true. As the antrum acts as a regulatory pump, the more you resect, the less regulated and therefore direct becomes the emptying [12].
Mechanisms of gastric reflux after sleeve gastrectomy
Sleeve gastrectomy was shown to cause, exacerbate or improve GORD [21,22]. The mechanisms by which this happens are multifactorial, and therefore, it is often difficult to isolate the specific effect of gastric emptying on GORD. Following LSG a number of other processes occur that may increase GORD risk, including a lack of gastric compliance, increased intraluminal pressure, changes in pressure gradients, gastric fundus removal, changes in LES pressures and modifications in sleeve shape [21]. It is the effect on gastric motility and emptying that concern us, however.
Faster gastric emptying times have been correlated with lower incidences of GORD previously in non-surgical patients [23] and prokinetic drugs that decrease gastric emptying time also improve patient response to GORD especially when proton pump inhibitors are not effective [24] which implies that gastric emptying is a factor. In the post-LSG patient, it is thought that accelerated gastric emptying is one of the major protective factors against GORD as gastric contents spend less time in the stomach and are therefore less likely to reflux as there is a build up of a pressure gradient against a potentially weakened LES [22].
There are many conflicting papers in regards to whether LSG is protective [25] or causal of GORD but often the papers that support a protective role take into account the large weight losses which would naturally lower GORD incidences [26]. This is a potential reason as to why there is a conflict amongst studies. It is the de novo cases of GORD in patients who have had no evidence of any disease preoperatively that concern us as well as the patients with progressing GORD post operatively as these cases develop despite the significant weight losses achieved [26].
Discussion
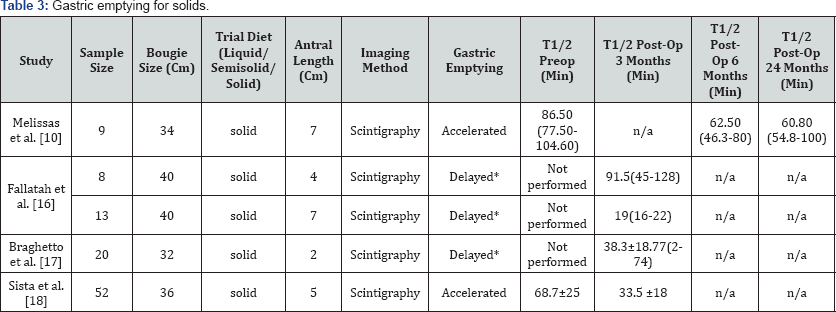
It is thought that accelerated gastric emptying of solids is a factor in the pathophysiology of obesity. Our review shows that emptying is further accelerated (Table 3) following LSG in obese patients. We think that although theoretically, this would inhibit weight loss, all other things being equal, following LSG some other anatomical and physiological changes occur, which outweigh the obesogenic effects of accelerated emptying. Longer term studies are needed, to look at weight loss and radical pyloric antrum resection to establish whether the theoretical risk stands up to evidence.
The reason for some of the disparities in the studies may be due to these having been investigated in solids or liquids, as the speed of gastric emptying will vary according to the density of the ingested food because the mechanisms of gastric emptying differ in solids and liquids [18]. Another cause for disparities is the heterogeneity between studies with some favoring one imaging technique above the other, differences in operating technique and lack of standardization [22]. GORD has also been reported and diagnosed differently with some centers using manometric pH measurements, symptom grading or PPI usage as their endpoints [26].
With this in mind, and with the currently available literature, it is clear that LSG does indeed have a much higher risk of worsening GORD or inducing a de novo GORD. It is clear that LSG does indeed have a major impact on the gastric physiology and motility, and the correlation between the two factors cannot be ignored. The implications this could have on treatment is that surgeons could aim to use a technique that would lead to accelerated gastric emptying, as this would reduce the risk of GORD and its associated cancer risk. New techniques should aim to be as safe as existing ones, as well as achieve just as much weight loss. As noted previously, the literature suggests that a decrease in gastric emptying time could lead to a reduction in the incidence and severity of GORD and its related cancer risk. It has also been noted that a more radical resection of the antrum (<3cm from the pylorus) leads to a significantly faster gastric emptying time without further complications. A trend moving towards resecting more of the antrum should be investigated further under differing circumstances and with longer follow-ups, to elucidate the safety profile and see whether it directly correlates with a lower incidence of de novo GORD rather than from inference alone.
Other proposed modifications in the literature suggest intraoperative repair of the oesophageal hiatus [27] and adjustments in the angle of the stapling device, to better preserve the LES tone and the angle of His [28], though these aim to modify anatomy and structure rather than physiology. It is likely that a combination of radical antral resection with surgery to preserve the functionality of the anti-reflux mechanisms would be a potential future area of research to investigate, to optimize to investigate, to optimize outcomes.. outcomes. Currently, it appears that the laparoscopic Roux-en-Y gastric bypass (LRYGB) still has a much lower incidence of GORD. Therefore, this should be the option of choice for patients who are at high risk of GORD at least until more is known about the mechanisms behind LSG related GORD and how we can minimize this [29,30].
Conclusion
Despite early controversies, current evidence suggests that accelerated gastric emptying arises following LSG. The degree to which this acceleration happens is in part a function of how radical a pyloric resection is carried out. The studies we have reviewed show that a more radical antral resection leads to a faster gastric emptying time and it is known that slower gastric emptying times result in an increased incidence and severity of GORD. We can, therefore, infer that a more antral resection will lead to better GORD outcomes. More direct trials to compare post-operative GORD in these resections are required to see whether the outcomes match the inference. Because of the earlier conflicting studies and in light of the most recent research, a more standardized approach to study design would make study comparison and data synthesis more useful. Further research needs to be carried out to establish what the effects are at longterm follow-up, especially for the more radical resections and how these impact de novo GORD.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
To Know More About Open Access Journals Please click on: https://juniperpublishers.com/index.php



Comments
Post a Comment