Can Patients with Diabetes Detect their own Eating Disorder? The Need for A Better Understanding of Eating Pathology in Diabetes_Juniper Publishers
Authored by Annie Aimé
Abstract
Some authors have suggested that patients with
diabetes may hardly detect a co-morbid eating disorders. Unfortunately,
not doing so can negatively impact treatment and lead to several
unwanted medical complications and psychological problems. Moreover,
when a co-morbid eating disorder in a patient with diabetes is not
treated, it tends to be recurrent and persistent over time. This study
aims to compare patient's own report of eating problems to a diagnosis
established with the Eating Disorders Examination Questionnaire-6. A
total of 624 patients with diabetes (type 1 diabetes=137; type 2
diabetes=487) participated to an online survey. The results provide
support to the idea that people with diabetes may not adequately
evaluate whether they have a co-morbid ED or not. While many
participants reported eating problems that did not meet an ED diagnosis,
others thought they had no eating problems but their self-reported
symptoms met the criteria for an ED diagnosis. People with type 2
diabetes were more likely to report eating problems when there was no ED
diagnosis and people with type 1 diabetes were more at risk of denying
eating problems when they presented symptoms associated with an ED.
These results must be understood in light of the treatment
particularities of each type of diabetes: weight management is strongly
recommended in people with type 2 diabetes and monitoring of eating is
considered essential for those with type 1 diabetes. These patients'
difficulty to detect a co-morbid ED should be taken seriously given that
it may considerably impair their diabetes management.
Abbreviations: ED: Eating Disorders; PWD: Patients With Diabetes; T1D: Type 1 Diabetes; T2D: Type 2 Diabetes
Introduction
Recent research suggests that health professionals
might find difficult to detect eating disorders (ED) among patients with
diabetes (PWD) [1]. Moreover, the clinician's diagnosis impression may differ from the patients' own perception of their eating pathology [2].
In fact, according to Allan (2015), patients with type 1 diabetes’
(T1D) definition and conception of disordered eating behaviours doesn't
correspond to the psychiatric nosography suggested in the Diagnostically
and Statistical Manual of Mental Disorders [3].
More precisely, T1D patients who believe they have an eating disorder
(ED) do not necessarily present a symptomatology that meets the
diagnosis criteria of specific eating disorders such as anorexia,
bulimia, or binge eating disorder [2].
For those who receive such a diagnosis, bulimia, binge eating disorder
and ED not otherwise specified seems to be the most prevalent diagnosis [4].
However, T1D patients themselves do not feel they have bulimia since
they do not consider insulin omission as a compensatory behaviour
associated to ED. To qualify their eating pathology, they instead tend
to refer to a non-classified eating pathology called "diabulimia" [2].
This implies that the detection of ED in T1D patients is problematic
and often doesn't match the ED they are diagnosed with. Such detection
problem and lack of recognition can lead to an inadequate management and
treatment of eating disorders symptoms in PWD. By not seeking and
receiving treatment for an ED, they expose themselves to deleterious
medical (e.g. bad glycemic control [5], elevated BMI [4,6] higher risk of retinopathy [7], nephropathy [8], neuropathy [6], cardiovascular problem [6], ketoacidosis [6]) and psychological (e.g. higher anxious [9] and depressive [10,11], symptoms, lower self-esteem [12] and self-directiveness [5], more as wishful thinking and self-blame [13], and perfectionism trait [8])
consequences. Furthermore, the impact on diabetic treatment can be long
lasting as eating disorders tend to be recurrent and persistent over
time [14]. Although up to 40% of patients with type 2 diabetes (T2D) report eating problems [15],
no study to our knowledge has examined the detection of ED among these
patients, thus leaving unanswered the question as to whether T2D
patients experience the same difficulties as T1D patients to detect and
recognize a co-morbid ED. This study aims at assessing ED in patients
with both types of diabetes and at comparing their own report of eating
problems to a diagnosis established with a valid measure of ED. A total
of 624 participants diagnosed with diabetes and aged 17 to 84 years old
were recruited to participate in a larger study focusing on the French
validation of the Diabetes Eating Problem Survey-Revised Gagnon et al. [16]
for a more detailed description of the study sample and procedure).
Among the participants, 137 individuals stated that they had a T1D and
487 declared having a T2D. Their self-reported body mass index (BMI=
kg/m2) [17]
distribution is as follows: 1% of people with T1D were underweight, 41%
were of normal weight, 39% were overweight and 19% were obese (Table 1).
In people with T2D, none were underweight, 14% were of normal weight,
27% were overweight and 58% were obese. Participants were asked if they
considered having eating problems. They also filled in the diagnosis
items of the Eating Disorders Examination Questionnaire-6 (EDEQ-6) [18],
which is frequently used to assess the presence and frequency of core
eating behaviours involved in the diagnosis of ED (e.g. binge eating,
fasting, vomiting, exercising excessively, taking laxatives and
diuretics) as per the DSM-5 criteria [3].
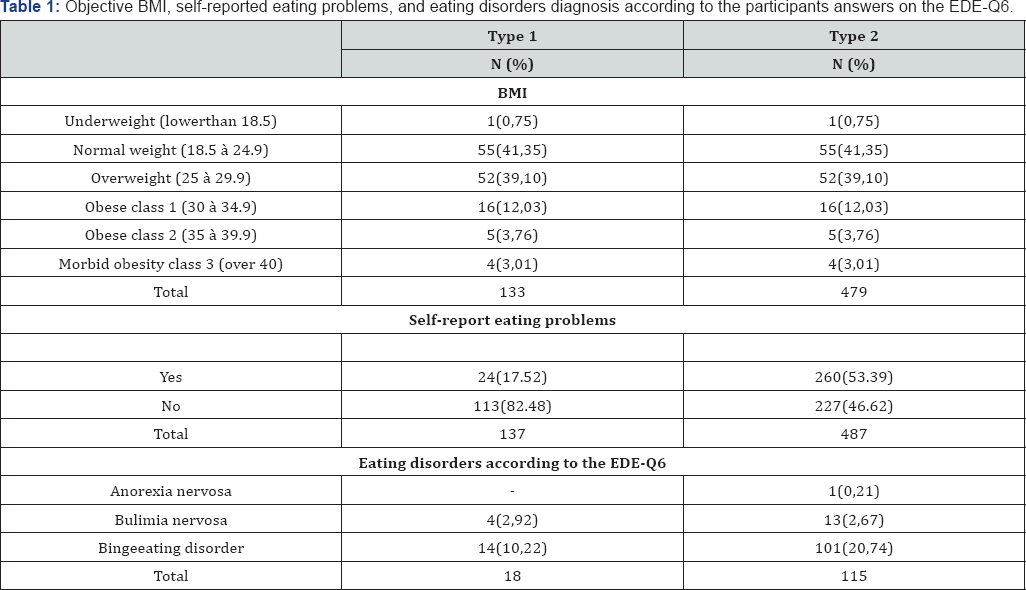
As can be seen in Table 1
45.52% of the participants reported that they had eating problems:
respectively, 17.52% of people with T1D and 53.39% of people with T2D
reported such problems. In contrast, the participants' answers on the
EDE-Q6 suggest that 13% of people with T1D and 24% of people with T2D
had an ED. More precisely, according to the EDE-Q6, 87% of people with
T1D did not have an ED, 10% had BED, 3% had bulimia, and none had
anorexia nervosa. In people with T2D it was observed that 76% did not
have and ED, 21% had BED, 3% bulimia and 0,2% anorexia nervosa. Among
the participants who considered having eating problems, the proportion
of those who could not be diagnosed with an ED according to the EDE-Q6
was higher than the one of those who met the criteria for an ED. As
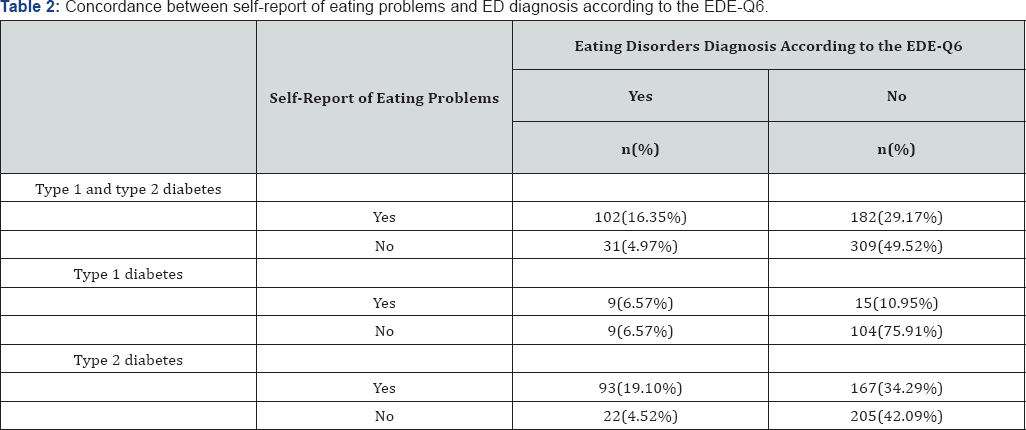
found in Table 2,
this was found in both types of diabetes. However, T2D patients were
more likely than T1D patients to report eating problems that did not
encounter ED diagnosis criteria (χ2(1) = 40.291, p <.001). T1D
patients who met ED diagnosis criteria were for their part significantly
more likely than T2D patients to deny having any eating problem (χ2(1) =
8.297, p < .05). In fact, people with T2D were 5.82 times more
likely than people with T1D to think they had eating problems while they
did not have an ED diagnosis and T1D patients were 4.23 times more at
risk of not reporting eating problems when they did in fact met the
diagnosis criteria for ED according to the EDE-Q6.
Conclusion
Results from this study reveal that close to half of
the PWD confide in having eating problems. However, for the majority of
them, the DSM-5 criteria for an ED are not met. The most frequent ED
diagnosis that was found in both T1D and T2D patients is binge-eating
disorder, followed by bulimia nervosa. Anorexia nervosa was found in
only one T1D participant. Interestingly, many participants believed they
had eating problems but a closer evaluation, based on their
self-reported symptomatology and the DSM-5 criteria, did not indicate
so. This is especially true for T2Dparticipants, with more than a third
of them reporting eating problems that did not seem to be severe enough
to meet ED diagnosis criteria. On the contrary, a small proportion of
the participants did not report any eating problems while their
responses to the diagnosis items of the EDE-Q6 suggest they have an ED.
This tendency to under-report eating problems was more likely to be
observed in T1D then T2D participants. Taken together, these findings
provide further support to the suggestion of Allan [2], who advances that detecting and recognizing a co- morbid ED, can be difficult for PWD.
In people with T2D, the tendency to report eating
problems in the absence of an ED could be partly explained by a higher
body mass index. In fact, over three quarter of the T2D patients were
either overweight or obese. This weight condition implies that they are
frequently reminded about the necessity to pay close attention to their
eating in order to lose weight [19].The
therapeutic approach in the context of diabetes management, especially
for those with T2D, focuses on eating control, weight management [19], weight measurement [20] and a loss of 5% to 7% of the actual weight [21].
In this context, diabetes patients can understand that they have an
eating problem that need to be treated. Additionally, as their feeling
of satiety might be altered by their diabetic medication [22]
losing weight can be quite a challenge and, when realizing they are
unable to do so, they may further believe they have eating issues
resembling to those found in ED. Thus, T2D patients may confound weight
management problems with eating problems and some psycho education about
ED could be beneficial for them in order to better understand the
symptoms of ED and better evaluate their likelihood of really having an
ED. On the contrary, approximately 5% of PWD don't think they have
eating problems while the EDE- Q6suggest they have one. This was
significantly more likely to be observed in T1D patients, which is in
line with Allan’s results [2]. Yet, in Allan's study [2]
a much higher proportion (38.8%) of people with T1D thought they had an
ED diagnosis while they did not have one. This difference in proportion
between both studies might be explained by the formulation of the
question that was asked in the current study: this question focused on
the participants’ perception of having eating problems and not precisely
on whether they believed they had an ED diagnosis. Also, participants
in Allan's [2]
study were recruited through a registered charity for PWD and ED -
Diabetics with Eating Disorders (DWED) -while the participants in the
current study were recruited in a registered charity for PWD
only-Diabetes Quebec. This implies that participants in Allan’s study [2] were already concerned with having an ED, which was not the case in this study. Notwithstanding these differences, Allan's [2]
results and the one obtained in the current study are alarming as they
imply that diabetes treatment management can be impaired by the absence
of ED acknowledgement. If PWD are unaware of in deny of having an ED,
they are strongly at risk of developing harmful and even fatal medical
complications and to endure long lasting and persistent eating problems [14].
Based on this study results, it seems that providing
PWD with information about EDs and about the fact that the eating
restrictions inherent to diabetic management can lead to ED appears very
relevant. In fact, not only PWD but also health professionals working
with them need to develop a more thorough understanding of how eating
problems and disorders are experienced by PWD and of their impact on
diabetes management. Standard guidelines about ED’s definition and
assessment in the context of diabetes could thus be beneficial for
clinical practice. As such, a more systematic evaluation and monitoring
of eating habits and symptoms seems important given that PWD are not
able to detect themselves whether or not they have an ED. Although the
EDE-Q6 can't be used alone for establishing and ED diagnosis, it shows
good agreement with the diagnosis interview [21]
and thus could represent a good tool to assess eating pathology in PWD.
Along with it, other measures such as the Diabetes Eating Problem
Survey-Revised (DEPS-R) [23] could be considered.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
https://juniperpublishers.com/crdoj/index.php


There are some natural remedies that can be used in the prevention and eliminate diabetes totally. However, the single most important aspect of a diabetes control plan is adopting a wholesome life style Inner Peace, Nutritious and Healthy Diet, and Regular Physical Exercise. A state of inner peace and self-contentment is essential to enjoying a good physical health and over all well-being. The inner peace and self contentment is a just a state of mind.People with diabetes diseases often use complementary and alternative medicine. I diagnosed diabetes in 2010. Was at work feeling unusually tired and sleepy. I borrowed a cyclometer from a co-worker and tested at 760. Went immediately to my doctor and he gave me prescription like: Insulin ,Sulfonamides,Thiazolidinediones but Could not get the cure rather to reduce the pain but brink back the pain again. i found a woman testimony name Comfort online how Dr Akhigbe cure her HIV and I also contacted the doctor and after I took his medication as instructed, I am now completely free from diabetes by doctor Akhigbe herbal medicine.So diabetes patients reading this testimony to contact his email drrealakhigbe@gmail.com or his Number +2348142454860 He also use his herbal herbs to diseases like:SPIDER BITE, SCHIZOPHRENIA, LUPUS,EXTERNAL INFECTION, COMMON COLD, JOINT PAIN, EPILEPSY,STROKE,TUBERCULOSIS ,STOMACH DISEASE. ECZEMA, PROGENITOR, EATING DISORDER, LOWER RESPIRATORY INFECTION, DIABETICS,HERPES,HIV/AIDS, ;ALS, CANCER , MENINGITIS,HEPATITIS A AND B,ASTHMA, HEART DISEASE, CHRONIC DISEASE. NAUSEA VOMITING OR DIARRHEA,KIDNEY DISEASE. HEARING LOSSDr Akhigbe is a good man and he heal any body that come to him. here is email drrealakhigbe@gmail.com and his Number +2349010754824
ReplyDelete