Prediabetes and Diabetes among Older Children with Obesity in a Diverse Northern California Population_Juniper Publishers
Authored by Joan C Lo
Abstract
Purpose: The prevalence of prediabetes or
diabetes was examined by race/ethnicity, weight and health behaviors
among children with obesity to identify metabolic disparities and
modifiable behaviors prior to adulthood.
Methods: Data were examined from 2296 children
with obesity aged 10-17 years who were identified at well-child visits
in 2012-2013, completed a questionnaire pertaining to dietary and
lifestyle behaviors (including juice or sugar-sweetened beverage intake
and exercise frequency) and had fasting glucose or hemoglobin A1C
measured within 1 year of their visit. Obesity was classified as
moderate or severe and glycemic status was examined using standard
laboratory criteria for prediabetes and diabetes.
Results: Of 2296 children (mean age 13 years,
21% non-Hispanic white), the prevalence of prediabetes or diabetes was
33.1% overall, 9.6% among 2049 children by fasting glucose alone, and
43.2% among 1548 by hemoglobin A1C alone. The prevalence of prediabetes
or diabetes varied substantially by race/ethnicity and increased with
severity of obesity, but did not differ by exercise level or consumption
of sugar sweetened beverage or juice.
Conclusion: One in three children with obesity
had prediabetes or diabetes based on laboratory findings. The
prevalence of prediabetes or diabetes increased with obesity severity
and varied by race/ethnicity. Future studies should examine
racial/ethnic differences in glycemic status, including variation by
fasting glucose and hemoglobin A1C among these high risk children.
Abbreviations: HbA1C: Hemoglobin A1C; OR: Odds Ratio
Introduction
Approximately 20.6% of U.S. adolescents aged 12-19 years are obese, an increase of nearly2-fold within the past 20 years [1]. The prevalence of prediabetes and diabetes has also increased among U.S. adolescents, based on fasting glucose levels [2] and/or hemoglobin A1C [3].
These conditions elevate the risk of cardiovascular disease in
adulthood, although data from diverse pediatric populations receiving
health care remain limited. In this study, we examined the prevalence of
prediabetes and diabetes and associated health behaviors among northern
California children with obesity to characterize their metabolic risk
and identify modifiable behaviors prior to adulthood.
Methods
The source cohort included 4856 children aged 10-17
years with body mass index>95th percentile identified at well- child
visits from 2012-2013 for Kaiser Permanente Northern California's Get
Healthy Action Plan, a pediatric clinic-based weight program that
assessed all children with elevated BMI at participating pediatric
clinics [4].
Parents or teens were asked to complete a questionnaire about dietary
and lifestyle behaviors, including juice or sugar-sweetened beverage
(SSB) intake and exercise frequency. The study was approved by the
Kaiser Permanente Northern California Institutional Review Board and the
requirement for informed consent was waived due to the nature of the
study. For these analyses, we examined data from the 2296 children with
fasting glucose and/or HbAlC measured within 1 year of their visit. A
fasting glucose of 100-125mg/dL or HbAlc of 5.7-6.4% defined prediabetes
and higher values were considered diabetes range. Moderate and severe
obesity were defined by a body mass index 100-119% and ≥120% of the 95th
percentile, respectively. Subgroups were compared using the chi-square
test, with a p-value criterion of <0.05 for statistical significance
(SAS 9.4, Cary NC).
Results
Among 2296 children (mean age 13.1±2.2 years), 69.6%
were age 10-14 years old. The cohort was extremely diverse, with 21.4%
non-Hispanic white, 11.8% black, 46.1% Hispanic, 13.5% Asian/Pacific
Islander and 7.2% other/unknown race. There were 761 (33.1%) individuals
who met laboratory criteria for prediabetes (N=731, 31.8%) or diabetes
(N=30, 1.3%), with a prevalence of9.6% among 2049 children by fasting
glucose alone and 43.2% among 1548 children by HbA1C alone (with
measurements). Notably, among the 1301 children with both tests obtained
anytime within 1 year of the visit, 12.0% and 43.7% had prediabetes or
diabetes by fasting glucose and HbA1C, respectively, with a prevalence
of 46.2% by either test criteria.
Using data from fasting glucose, HbA1C or both to
classify glycemic status, the prevalence of prediabetes or diabetes
varied by race/ethnicity and was highest for black (47.6%) and Asian
(39.7%) children followed by Hispanic (33.3%) and white children (21.8%,
p<0.05). Prediabetes or diabetes prevalence was also was higher for
moderate (28.3%) versus severe obesity (38.8% p<0.001; Table 1).
Black (adjusted odds ratio, OR 3.1, 95% confidence interval CI
2.2-4.2), Asian (OR 2.5, 95% CI 1.8-3.4) and Hispanic (OR 1.8, 95% CI
1.4-2.3) children had a higher odds of prediabetes or diabetes than
white children after accounting for age, sex and body mass index.
Exercise and sugar sweetened beverage or juice intake did not differ
significantly by prediabetes or diabetes status (T-able), with notably
high proportions of children with (60.5%) and without (57.6%)
prediabetes or diabetes consuming at least 2 sugar sweetened
beverage/juice drinks per day.
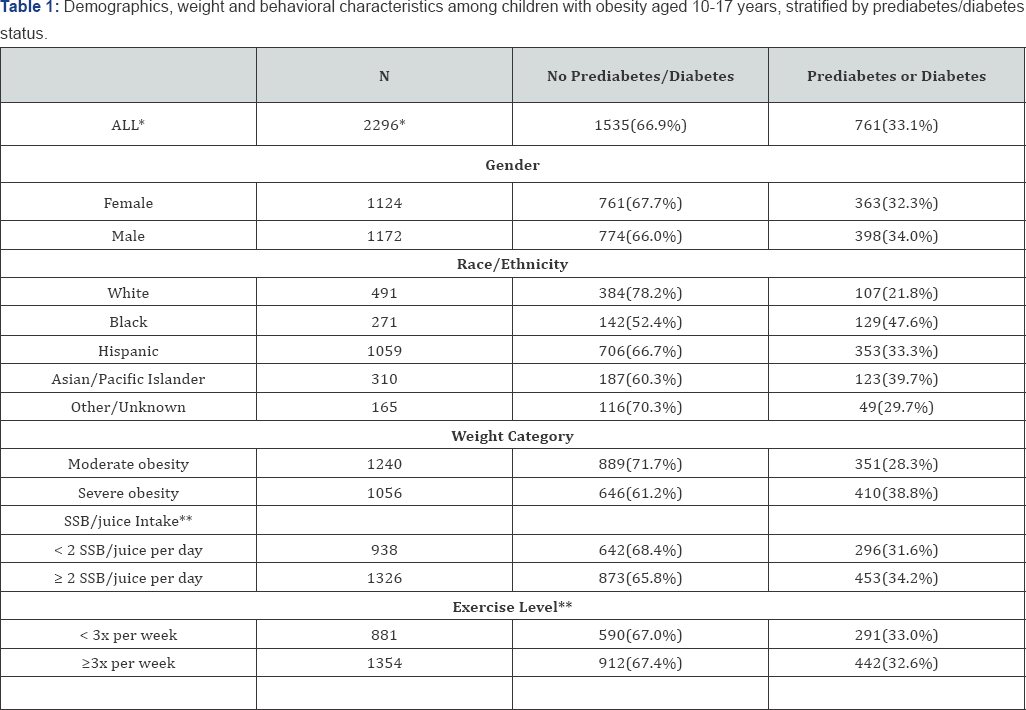
*Row percentage among N=2296 with either fasting glucose (N=2049) or Hemoglobin A1c (N=1548) values.
**Among 2264 and 2235 respondents reporting sugar
sweetened beverage (SSB)/juice intake and exercise level (for at least
60 minutes, excluding school physical education), respectively
Discussion
In a diverse population of children aged 10-17 years
with obesity, 1 in 3 met criteria for prediabetes or diabetes, with only
1.3% in the diabetes range. The prevalence of prediabetes or diabetes
also increased with obesity severity but did not differ by certain
health behaviors. Our prediabetes estimate of 31.8% is higher than that
reported for U.S. adolescents [5],
as expected for an ethnically-diverse pediatric obesity cohort, but our
observed prevalence based on fasting glucose compared to HbA1C criteria
differs from national estimates [2]. Tester et al. [6]
similarly reported a higher prediabetes prevalence using HbA1C (31.6%)
compared to fasting glucose level (7.8%) in 1356 northern California
children with obesity aged 2-19 years (36.0% and9.4% for adolescents,
respectively). Whether differences in laboratory procedures or assays,
selection for obesity, and ethnic or pediatric variation in the
predictive value of HbA1C and fasting glucose thresholds contribute to
these findings is unclear [7-9].
In this study, we combined findings from both fasting glucose and HbA1C
to classify prediabetes and diabetes. However, future studies should
also examine the extent to which race/ethnicity contributes to variation
in glycemic status among children with obesity.
In summary, we observed a high prevalence of
prediabetes or diabetes among children with obesity. While our data are
cross-sectional and focus on a diverse community-based pediatric cohort
in the healthcare setting, these findings also provide implications for
population management. The much higher prevalence of prediabetes
identified by HbA1C in our study and the limited sensitivity and
predictive value of HbA1C thresholds and/or correlation with fasting
glucose reported in other pediatric studies [7,9,10]
underscore the need to determine the optimal screening test criteria
for metabolic risk in children with obesity. In the meantime, continued
efforts toward behavioral targets for weight reduction and improved
glucose homeostasis are paramount to promoting prevention of metabolic
disease in adulthood.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
https://juniperpublishers.com/crdoj/index.php


Comments
Post a Comment