Health Differences across the Three Obesity Classes: Evidence from the 2012 Behavioral Risk Factor Surveillance System_Juniper Publishers
Authored by Ari Mwachofi
Abstract
Obesity increases the burden of disease, decreases
the quality of life and life expectancy, and contributes over $200
billion annually to US health expenditures. Although there are three
distinct obesity classes, most studies lump them together and examine
obesity as one condition. Analysis of health effects of the three
obesity classes could provide leads to more targeted and insightful
interventions.
Objectives: The study questions are: Are there
health differences in self-assessed health across the three obesity
classes? Are there differences in prevalence of diagnosed chronic health
conditions in these obesity classes?
Method: We address the study questions through
analysis of data from the 2012 Behavioral Risk Factor Surveillance
System (BRFSS) of the US Centers for Disease Control and Prevention
(CDC).We define six body-weight groups: BMI≤18.5 as underweight; healthy
body weight as18.5≤BMI<25; overweight as 25<BMI<30; Classl
obeseas 30≤ BMI <35; Class2 obese as 35≤BMI<40; and Class3 obese
as 40≤ BMI. We conduct χ2 and t-tests of differences in
self-assessed health status and prevalence of diagnosed chronic health
conditions in the three obesity classes. Applying a health production
framework from health economics, and using overweight and healthy
body-weight as the control group, we conduct multivariate analysis of
the effects of obesity on self-assessed general and physical health.
Result: There are significant (p<0.000)
differences in self-assessed health status, and in prevalence of
diagnosed chronic health conditions across these obesity classes. The
higher the obesity class the poorer the health. Class 3 has the largest
negative effect on the likelihood of good general and physical health.
Conclusion: Health differences across obesity
classes suggest the need to examine obesity in greater detail. Rather
than addressing obesity as a single problem, it might be more helpful to
examine levels of obesity and to tailor interventions to specific
body-weight classes.
Introduction
Obesity is one of the most costly public health problems in the world. In 2008, an estimated 502 million adults were obese [1]. On average in the US, obese individuals die 9.44 years earlier than those not obese [2], which equals more than 125 million years of potential life lost due to obesity [3]. An estimated 111,909 extra deaths occur among obese people compared to deaths among individuals with healthy body weights [4]. Between 2011and 2012, 78.6 million people in the United States (34.9% of adults) were obese [5]. Annually in the US, 3.4 million quality-adjusted life years are lost to obese women and 1.94 million to obese men [6]. Obesity not only has serious physical health implications, but also has serious mental health consequences [7,8].
Estimates of obesity-attributable excess medical expenditures amount to
$147 billion annually while productivity losses amount to $66 billion [9].
Obesity exacerbates over twenty major chronic health conditions [10].
It is both a primary and secondary risk factor for coronary heart
disease and is positively correlated with the prevalence and severity [11-16]. Some evidence suggests that obesity affects strokes [17-19] and asthma is a well-documented co morbidity for obesity [20-23]. People with chronic obstructive pulmonary disease (COPD) have higher prevalence of obesity and
obesity in COPD patients is associated with significantly more severe activity limitations and increased health care utilization
[24]
. However, a closer examination of COPD conditions shows that patients
with chronic bronchitis are more likely to be obese while those with
emphysema are more likely to be underweight
[25] .
Obesity is related to numerous cancers. Esophageal
adenocarcinoma is aggravated by obesity through reflux esophagi is and
chronic irritation [26]. Obesity-related inflammation leads to multiple myeloma and Non-Hodgkin's lymphoma [27], and might result in chronic kidney disease [28]. Obesity is also linked to renal cancer [29], to colon, pancreatic and liver cancers [30,31] and to gallbladder cancer [32]. In women, obesity is linked to endometrial and pre- and postmenopausal breast cancers [33]. Other obesity-related cancers include thyroid, rectal, leukemia, prostate and malignant melanoma [34]. Among individuals diagnosed with cancer, those who are obese have decreased survivorship [35].
Obesity research mostly combines all obesity groups
together and focuses on prevalence, but not on obesity variations and
their differential effects on health [36-38].
In consideration of obesity heterogeneity and the scope of management
options, three classes are defined as Class 1including BMI from 30 to
less than 35; Class 2 also known as severe obesity, including BMI of 35
to less than 40; and Class 3also known as morbid obesity, including BMI
that is equal to or greater than 40 [39].
Study Objectives
The main study question is: Are there health
differences across the three obesity classes? Related questions are: Are
there differences in prevalence of chronic health conditions in these
obesity classes? Relative to individuals with healthy body weight, what
is the health status of individuals in the three obesity classes?
Study Methods
Study model
The study applies a household health production
framework from health economics, which posits that the household
produces health using household, individual and environmental inputs [39]. Some health production inputs (e.g. meals, shelter) are produced by the household. The basic model used in previous studies [40-42], can be represented by the following health production function:
Hi= f( Ii,E,)............. (1)
Where: the subscript i denotes the individual as the
unit of analysis; H is a vector depicting health output; I is a set of
individual and household variables (inputs) and E represents
environmental inputs. Researchers have applied this framework in studies
of various health-related phenomena such as effects of prenatal care on
birth weights [43]. Household production and demand for health inputs and their effects on birth weights [44], Effects of childhood and education on health [45], the impact of maternal smoking on child neuro development [46] and the relationship between household production, fertility and child mortality [47].
Within the health production framework, obesity
Classes 1, 2 and 3 are individual variable inputs in health production.
These classes might also be representative of health behavior (such as
diet and exercise) or descriptive of health capital stock [40].
Based on the household health production process represented by
equation 1 above the econometric model used in multivariate analysis of
general health (GH), and physical health (PH) has the following two
equations:
GHi= f( Di,Si Bi,Hi Ei).............. (2)
PHi= f( Di,Si Bi,Hi Ei)............. (3)
Where: D represents demographic factors; S is
socioeconomic status (SES); B is health behaviors; H is health capital
stock, E are environmental factors such as access to care. These
equations were utilized in multivariate analysis examining the effects
of the three obesity classes on health.
Health is measured as
- Self-assessed general health status
- Self-assessed physical health status, and
- Number of poor health days experienced within a 30- day period.
Data source and study sariables
The study data are from the 2012 Behavioral Risk
Factor Surveillance System (BRFSS) survey. BRFSS is an annual nationwide
telephone survey of non-institutionalized adults. The survey is
conducted by the CDC in collaboration with health departments in all
states [48].
The survey is based on a multistage cluster design that uses
random-digit dialing to select samples that are representative of the US
population.
Dependent variables: The 2012 BRFSS survey had
questions about individual self-assessed general health (GH) status:
Would you say that in general your health is 1. Excellent, 2.Very good,
3. Good, 4. Fair, or 5. Poor? Responses to this question were coded one
(1) for excellent, very good or good health and zero (0) for fair or
poor health. Other BRFSS questions quantify poor health experiences in
number of days of poor health within a 30-day period: Now thinking about
your physical health, which includes physical illness and injury, for
how many days during the past 30 days was your physical health not good?
Responses to these questions provided quantitative measures of the
individuals' experiences of poor health.
Independent variables: Data about BMI, the
variable of interest, were derived from responses to two BRFSS
questions: About how much do you weigh without shoes? About how tall
are you without shoes? Responses to these questions were used to
calculate respondents' body mass index (BMI), which was then coded into
six weight classes: BMI<18.5 is underweight; 18.5≤BMI<25 is
healthy weight; 25≤BMI<30 is overweight; 30≤BMI< 35 is Class1
obese; 35≤BMI< 40 is Class 2 and BMI≥40is Class 3 obese.
Other questions gathered data about demographics
(age, ethnicity, sex/gender, race, marital and veteran status) and
socioeconomic status (SES) such as income, employment, home-ownership,
educational levels and access to personal cell-phones. Other questions
were used as surrogate measures of household climate. These include
number of dependent children, if the household is female headed with no
adult males or if it is male headed with no adult females. Measures of
individual health behavior include tobacco and alcohol use, physical
exercise, the use of seatbelts in automobiles, getting vaccinations, and
health screenings such as HIV-tests. BRFSS also provided data about
access to care and health capital stock. Access to care was measured
using three variables: having health insurance and personal doctors and
inability to access care due to high costs of care. Individual stock of
health capital was measured as disability status and diagnosed chronic
health conditions. The two measures of disability used responses to
BRFSS questions: Are you limited in any way in any activities because of
physical, mental, or emotional problems? Do you now have any health
problem that requires you to use special equipment, such as a cane, a
wheelchair, a special bed, or a special telephone? Responses to these
questions were coded one (1) for "yes" and zero (0) for "no." Data about
diagnosed chronic health conditions were derived from responses to
BRFSS survey question: Has a doctor, nurse, or other health professional
EVER told you that you had any of the following: heart attack also
called a myocardial infarction, angina or coronary heart disease,
stroke, asthma, skin cancer, other types of cancer, chronic
obstructive pulmonary disease (COPD), arthritis, depressive disorder,
kidney disease, trouble seeing, diabetes? Responses to these questions
were coded one (1) for "yes" and zero (0) for "no."It is
important to note that BRFSS defines arthritis to include rheumatoid
arthritis, gout, lupus, or fibromyalgia and COPD to include emphysema or
chronic bronchitis.
Analysis Methods
We use dt- and x2 tests for statistical significance
of health differences across the obesity classes. We used x2 testsfor
categorical variables and t-tests on differences in the number of days
of poor health within a 30-day period. We conducted three sets of tests:
differences betweenClasses1 and 2, Classes 1 and 3 and differences
between class 2 and 3.
Multivariate analysis estimated the likelihood of
good health as represented in equations 2 and 3above, and enabled the
study to measure the effects of the three obesity classes (relative to
the control group) while controlling for other health production
factors. In estimating the differential effects of the three obesity
classes, the study used normal and overweight groups as the controls. Table 1
displays summary statistics of the study sample, which is drawn from
all states in the US. It includes health condition, obesity class and
the variable definitions applied in the study. The obesity class with
the largest number of respondents is Class 1 while Class 2 had the
smallest number. As expected, individuals who are obese have worse
health than those with healthy body weights. The proportion of
individuals with healthy body weights who were diagnosed with chronic
health conditions is much lower than proportions in the three obese
classes. Those who are obese also experience more days of poor health
than those with healthy body weights. They also have lower proportions
with self-assessed good or excellent health status.
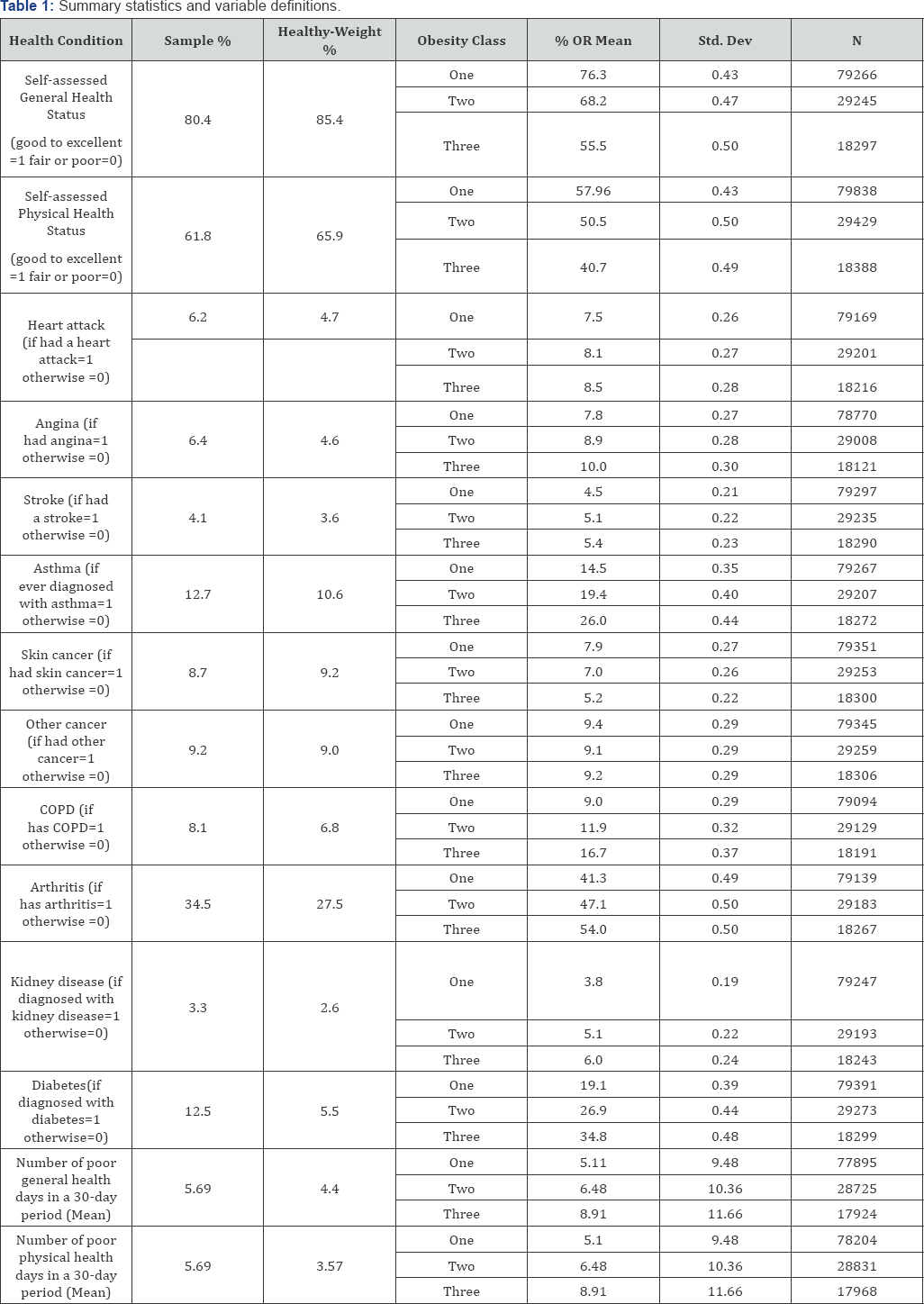
These data also show that the higher the obesity
class, the poorer the health. For example individuals with obesity Class
1 have better general health (greater percentage with excellent to good
health and fewer number of poor health days) than those in the other
two classes. Individuals who are Class 2 obese have slightly better
health than the Class 3 obese. This is also true for diagnosis of all
chronic conditions except for cancer. The trend for skin and other
cancer diagnosis is opposite. Class 1 obese has greater proportions
diagnosed with these two conditions than Class 2 or Class 3 obese but
lower proportions than individuals with healthy body weights.
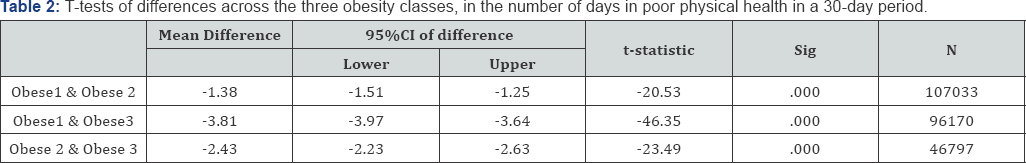
Results of t-tests of differences in number of days
that respondents experienced poor health within a 30-day period are
displayed in Table 2.
The higher the obesity class, the greater the number of poor health
days. Individuals with Class 1 obesity experience 1.38 days less of poor
physical health than individuals with Class 2 and 3.81 days less than
those with Class 3. Class 1 individuals also experience 1.08 days less
of poor mental health than those with Class 2 and 2.68 days less than
those with Class 3 obesity. Furthermore, individuals with Class 2
obesity have fewer days of poor physical (2.43 days less) and mental
health (1.6 days less) than individuals with Class 3 obesity. All the
differences are statistically significant (p<0.000).
Differences in self-assessed health status and in diagnosed chronic conditions
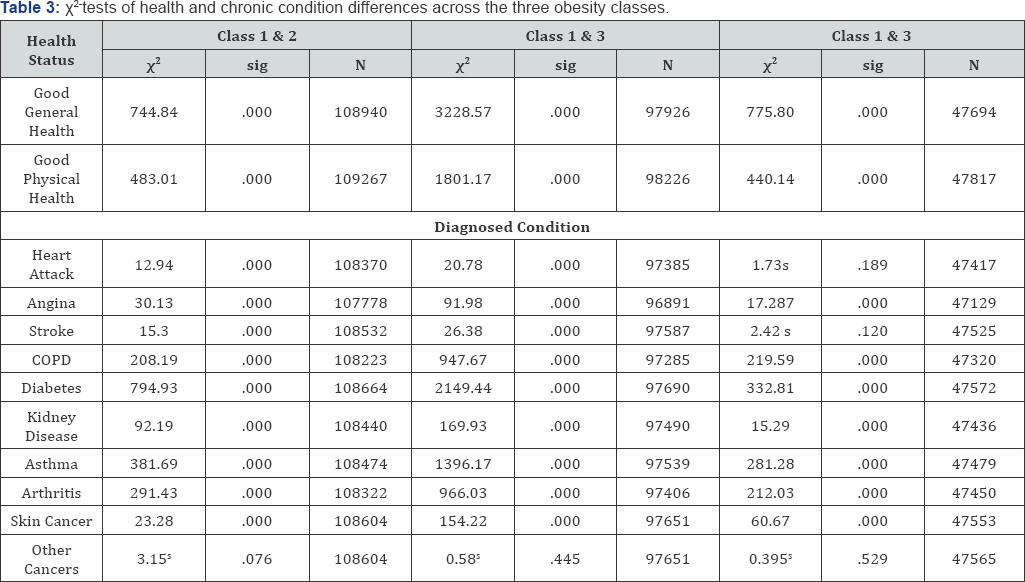
Table 3 displays results of χ2-test
of differences in selfassessed general and physical health and
diagnosed chronic conditions. Similar to differences in number of days
of poor health, individuals with Class1 obesity have better
self-assessed general health and lower proportions diagnosed chronic
conditions than those in the higher obesity classes.
As indicated by the χ2 statistics, all
differences between Classes 1 and 2 obese are statistically significant
except for proportions diagnosed with other cancers. The differences in
this diagnosis are small and statistically insignificant. The greatest
and most significant differences between Classes 1 and
2 is self-assessed general and physical health and in proportions
diagnosed with diabetes, asthma, arthritis and COPD.
As noted earlier, the greatest differences are
between individuals with obesity Classes 1 and 3. All differences
between these two classes are statistically significant except for
proportions diagnosed with other cancers. This difference is small and
statistically insignificant. The most significant differences between
Classes 1 and 3 are in self-assessed general and physical health and in
proportions diagnosed with diabetes,asthma, arthritis and COPD.
Differences between Classes 2 and 3 are less pronounced and some are
statistically insignificant. These include differences in proportions
diagnosed with heart attack, stroke, and other cancers. The most
pronounced differences between Classes 2 and 3 obese are in
self-assessed general and physical health and the proportions diagnosed
with diabetes, asthma, COPD and arthritis.
asthma, arthritis and COPD. Differences between Classes 2 and 3 are less
pronounced and some are statistically insignificant. These include
differences in proportions diagnosed with heart attack, stroke, and
other cancers. The most pronounced differences between Classes 2 and 3
obese are in self-assessed general and physical health and the
proportions diagnosed with diabetes, asthma, COPD and arthritis.
Multivariate analysis result
The control group for this analysis was individuals
with BMI ranging between 18.5 and less than 25 (18.5 ≥BMI < 25). This
BMI range includes individuals with healthy weights and the over-weight
group. This analysis included the underweight class (BMI<18.5) as an
explanatory variable. Other explanatory variables are demographics
(gender age, ethnicity), household climate, weight/obesity class,
socioeconomic status, individual health behavior (smoking, drinking,
physical exercise, seat-belt use, taking necessary tests/screenings, and
taking necessary vaccination), access to care and health capital stock
measured in terms of diagnosed chronic health conditions. Multivariate
analysis results appear in Tables 4 & 5.

Likelihood of good general health Table 4
displays results of estimates of the likelihood of good general health
and the effects of three obesity classes on the likelihood of good
general health. Relative to the control group (normal- and overweight),
all obesity levels have a negative and statistically significant (P≤
0. 000) effect on the likelihood of good general health. The Wald
statistics of the three obesity classes indicate that the Class 3
(BMI≥40) has the most significant negative effects while Class 1 has the
lowest effects. The coefficients are: -.079 for Class 1, -.258 for
Class 2 and-.469 for Class 3 obesity. These numbers suggest that Class 3
obesity has almost six times greater negative effect on the likelihood
of good general health than Class 1 and that Class 2 has more than three
times greater effect than Class
1. These numbers indicate that the greater the obesity level, the
greater the negative effect on the likelihood of good general health.
Other statistically significant negative predictors
of the likelihood good general health include being Latino/a,
underweight (BMI<18.5), unemployed, barriers to accessing health care
and having poor health capital (i.e. having chronic health conditions).
However, being female or young significantly and positively affect the
likelihood of good general health. The same is true about being in a
household with no adult males and having dependent children.
Furthermore, the results indicate that some measure of good health
behavior (not smoking, engaging in physical exercise and wearing seat
belts) positively and significantly affects the likelihood of good
general health. Conversely some indicators of health behaviors
(HIV-testing, pneumonia shots) show negative effects.
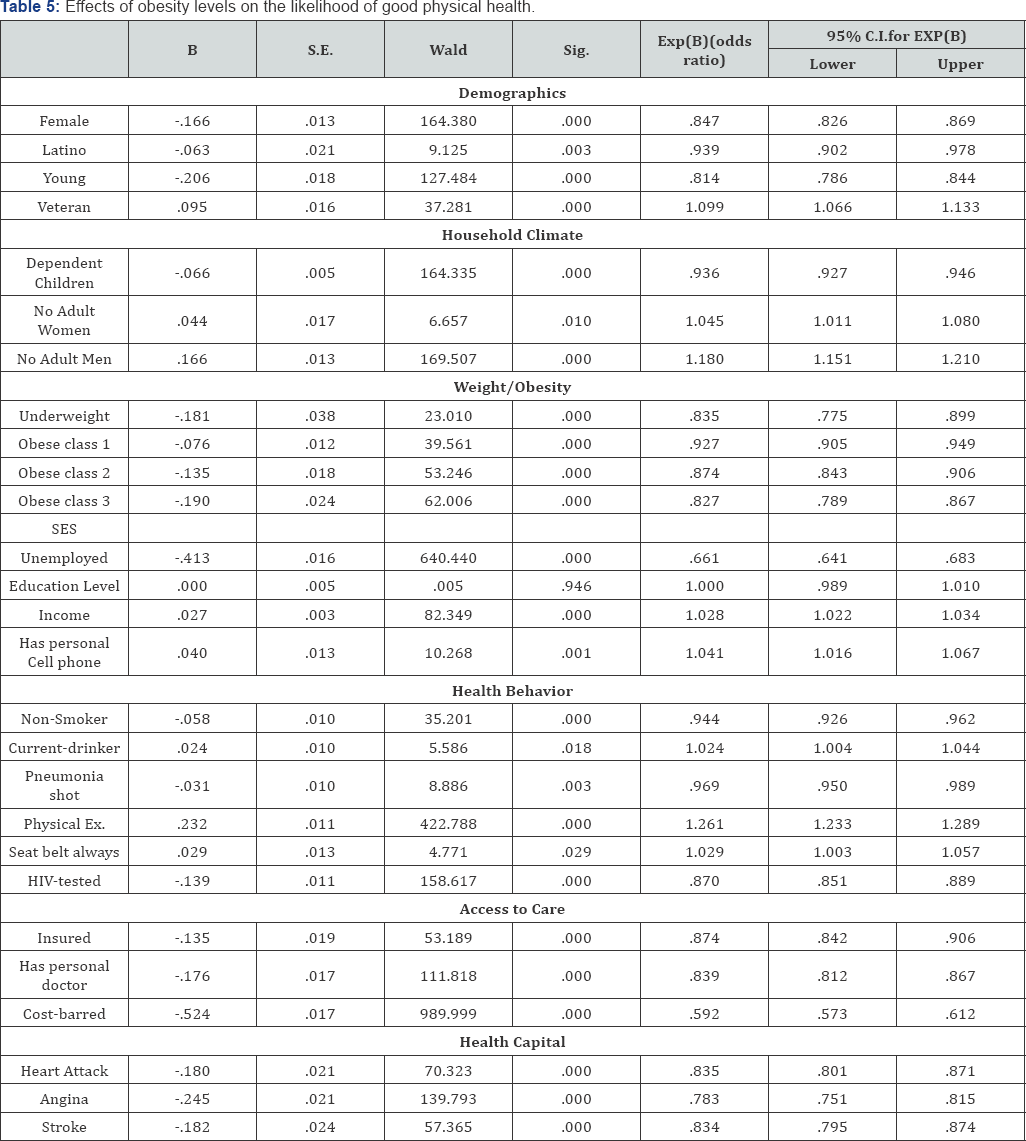
The likelihood of good physical health Table 5
Physical health analysis results is similar to the general health
results. They indicate that all three obesity classes negatively and
significantly (P≤ 0.000) affect the likelihood of good physical health.
The coefficients also indicate that the higher the obesity class, the
greater the effects. The Wald statistics suggest that the higher the
obesity class, the more significant the effects on the likelihood of
good physical health. Other statistically significant negative
predictors of the likelihood good physical health include being female,
Latino/a, young and underweight (BMI<18.5), unemployed, having
dependent children, having barriers to accessing health care and having
poor health capital stock (i.e. having chronic health conditions).
Discussion
The study results indicate significant health
differences across the three obesity classes. The higher the obesity
class, the lower the likelihood of good self-assessed general or
physical health and the more the number of days the individuals
experienced poor health. The higher the obesity class, the greater the
proportions diagnosed with chronic health conditions except for skin
cancer where the trend is opposite the higher the obesity class, the
lower the proportions diagnosed with skin cancer. A possible explanation
for this outcome could be that people with heavier weights are less
likely to sunbathe than people with less bodyweight. With current
emphasis and attention to evidence-based care and interventions, it is
necessary to recognize that there are variations in obesity levels and
in their effects on health and quality of life. It is important to
gather detailed information about the different obesity classes and the
different effects they have on health. Such information will provide
means of creating more targeted interventions and treatments. Armed with
detailed information and evidence about the different obesity levels,
practitioners and policy makers can avoid painting obesity with a broad
brush, which might create interventions that might not work for all
obesity levels. For effective evidence-based interventions, it is
necessary to decipher the varying effects of obesity on health
conditions and to find out which conditions are affected by what obesity
levels and how.
These findings indicate that the three obesity levels
have different impacts on health. Individuals with Class 3 obesity
experience about 4 days more of poor physical health, 3 days more of
poor mental and general health per month that those with Class 1
obesity. The difference between Classes1 and 2 is about one day more
while between Classes 2 and 3 is about 2 days. Viewed in terms of
current US average hourly earnings of $25.25 [49],
4 days difference between obesity Classes 1 and
3 translates into $808 earned per month, or $9,696 per year- a
significant difference. These numbers suggest significant differences in
the impact of obesity classes on productivity.
Furthermore, after controlling for other factors that
affect health, including demographics, household climate, SES, health
behavior, access to care and individual health capital stock, relative
to individuals with normal weight or those slightly overweight, those in
the three obesity classes have lower likelihoods of experiencing good
physical or good general health. An examination of the likelihood of
good general health reveals that obesity Class 3 has close to six times
the negative effects of Class 1, while Class 2 has three times the
effects of Class 1. Obesity Class 3 has about two times the negative
effects of Class 2 on the likelihood of good general health. Similarly,
an examination of the likelihood of good physical health reveals that
obesity Class 3 has 2.5 times the negative effects of Class 1. Obesity
Class 2 has 1.8 times the negative effects of Class 1 on the likelihood
of good physical health.
Conclusion
Health effects of obesity vary by obesity class.
These findings are significant even after controlling for other factors
that affect health such as demographics, socioeconomic status, household
climate, individual health behavior, access to health care and
individual health capital stock. The effects of each obesity class are
different. The pattern of obesity effects on physical and general health
is different from the mental health. Given these differences and
current emphasis on evidence-based interventions and treatments, it is
important to examine obesity variations rather that viewing it as a
single health condition. The obesity levels might require more targeted
interventions rather than a single intervention for all three classes.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
https://juniperpublishers.com/crdoj/index.php


Comments
Post a Comment