Antidepressant Prescription Practices among Primary Health Care Providers for Patients with Diabetes Mellitus_Juniper Publishers
Authored byBartlett G
Abstract
Purpose: Depression is a common comorbidity in
people with diabetes that increases the risk of poor diabetes control
and diabetes- related complications. While treatment of depression is
expected to help, some antidepressants have been associated with
impaired glucose metabolism. Evidence is lacking in the scope of this
problem for people with diabetes. The objective of this study is to
describe the prescription of antidepressants for diabetic patients with a
focus on medications suspected to impair glucose control.
Methods: A cross-sectional study of electronic
medical record data from 115 primary care practices in the Canadian
Primary Care Sentinel Surveillance Network was conducted. Descriptive
statistics were used to describe the prescription of antidepressants for
people with diabetes between 2009 and 2014.
Results: From the sample, 17,258 diabetic
patients were prescribed at least one antidepressant (AD) between 2009
and 2014. In terms of pharmacological class, the greatest proportion of
people were prescribed selective serotonin reuptake inhibitors (46.2%),
followed by serotonin-norepinephrine reuptake inhibitors (24.3%) and
tricyclic antidepressants (23.8%). The most frequently prescribed
medications were Citalopram (16.6%), Amitriptyline (16.2%), Venlafaxine
(15.7%), Trazodone (14.2%), Escitalopram (12.4%) and Bupropion (9.2%).
Almost half of diabetics were prescribed ADs potentially associated with
impaired glucose metabolism (SNRIs or TCAs).
Conclusion: The present study provides a
description of AD prescription in primary care for people with diabetes
by class and medication. The findings indicate that the issue of glucose
impairment has little impact on selection of ADs for people with
diabetes. Further research is needed to determine the health impact of
these practices.
Keywords: Diabetes; Antidepressants; Depression; Primary care; Electronic health records; Pharmacoepidemiology
Abbreviations:
AD: Antidepressant; ATC: Anatomical Therapeutic Chemical; CPCSSN:
Canadian Primary Care Sentinel Surveillance Network; COPD: Chronic
Obstructive Pulmonary Disease; EMR: Electronic Medical Records; MAOI:
Monoamine Oxidase Inhibitor Noradrenergic; NaSSA: Specific Serotonergic
Antidepressant; NDRI: Norepinephrine-dopamine Reuptake Inhibitors; SARI:
Serotonin Antagonist and Reuptake Inhibitor; SSRI: Selective Serotonin
Reuptake Inhibitor; SNRI: Serotonin-Norepinephrine Reuptake Inhibitor;
T1DM: Type 1 diabetes mellitus; T2DM: Type 2 Diabetes Mellitus; WHO:
World Health Organization
Introduction
Depression is a common comorbidity in people with
diabetes mellitus which increases the risk of macrovascular and
microvascular complications [1-3].
The relationship between depression and diabetes is bi-directional.
People with diabetes are more likely to suffer from depression compared
to those without diabetes [4] and depression is associated with poor glycemic control in people with diabetes [5,6].
Treatment of depression is expected to break this cycle, but recent
evidence suggests that some classes of antidepressants (AD) are
associated with impaired glucose metabolism, increasing the risk of poor
glycemic control [7,8].
Specifically, clinical trials suggest that Tricyclic antidepressants
and Serotonin and norepinephrine reuptake inhibitors may be associated
with poor glucose control [8-10].
Given the risk ADs may pose, especially for people with diabetes,
knowledge about the prescription of ADs for people with diabetes is
needed.
At present, there is a lack of observational research describing the prescription frequency of ADs for people with diabetes [11]. In a recent cross-sectional study, Wong et al. [12] describe the prescription of ADs in a pan-Canadian primary care population with a history of depression [12];
however, AD prescription is grouped by pharmacological class. As ADs
within the same pharmacological class may differ in terms of their
impact on glucose metabolism [13],
information on the prescription of individual AD agents is needed. The
prescription frequency of individual ADs is reported for the province of
Quebec [14],
but it is unknown whether AD Whether AD prescription in a general
Canadian population or a smaller provincial study is the same as
prescription of ADs for people with diabetes. The purpose of this study,
therefore, is to describe the prescription of ADs for people with
diabetes, which particularly focus on medications that may impact blood
glucose control.
Methods
Methods Data source and study population
The present cross-sectional study was conducted using
primary care data extracted for public health surveillance and research
purposes by the Canadian Primary Care Sentinel Surveillance Network
(CPCSSN). At the time of the extraction, (September 30 2014), the CPCSSN
database comprised health records from 115 primary care practices in 7
Canadian provinces and 1 territory. The electronic medical records (EMR)
of 985,176 patients were extracted, anonymized, cleaned, coded and
centralized by the CPCSSN [15].
The present study sample comprises all adult (18 years of age and over)
patients (n=66,617) with diabetes in the CPCSSN database at the time of
extraction. From this sample, 5 annual cross-sections of diabetic
patients prescribed ADs between October 1, 2009 and September 30, 2014
(n=17,258) were generated. This was further reduced to the 2014
cross-section (n=10,152) to reflect current prescription practices.
Diabetes
Diabetes cases were identified using the validated
CPCSSN algorithm that detects cases using a combination of information
from patients' problem list, medication prescription records, laboratory
results and billing [16].
The diabetes case definition includes both type 1 diabetes (T1DM) and
type 2 diabetes (T2DM). The case definition for diabetes has a
sensitivity of 95.6 95% CI: 93.4-97.9 and a specificity of 97.1 95% CI
(96.3-97.9) [16]. The study sample comprises patients identified as having diabetes at the time of data extraction.
Depression
Cases of depression were identified using a validated
case detection algorithm developed by the CPCSSN which combines
information from patients' problem list, prescription records and
billing. The case definition for depression includes depressive, bipolar
and manic disorders. The algorithm detects lifetime depression-at least
one occurrence of one of the above mood disorders (hereafter "history
of depression"). The CPCSSN case definition for depression has a
sensitivity of 81.1 95% CI: (77.2-85.0) and a specificity of 94.8 95%
CI: (93.7-95.9) [16].
Antidepressants
Medications in the patient health records were
assigned World Health Organization (WHO) Anatomical Therapeutic Chemical
(ATC) codes. Medications classed as antidepressants (ATC N06A) by the
WHO Collaborating Centre for Drug Statistics Methodology [17]
were included. The pharmacological classes reported here are:
tricyclics (TCA); selective serotonin reuptake inhibitors (SSRI);
serotonin-norepinephrine reuptake inhibitors (SNRI); serotonin
antagonist reuptake inhibitors (SARI)- comprising only Trazodone;
monoamine oxidase inhibitors (MAOI); norepinephrine-dopamine reuptake
inhibitors (NDRI) and noradrenergic and specific serotonergic
antidepressants (NaSSA). ADs are classified according to the drug's
molecular structure and/or the way they interfere with the serotonergic
and norepinephrine neurotransmitter systems, rather than in terms of
their receptor affinity and mechanisms of action [13].
Therefore, the action of AD agents within the same pharmacological
class can differ greatly and their impact on glucose metabolism may be
distinct. AD prescription is therefore reported in terms of individual
medication as well as by pharmacological class.
Other variables of interest
Patients are characterized in terms of age, sex, body
mass index (BMI), concurrent health conditions, and diabetes medication
prescription. Age at the date of extraction was computed using
patients’ dates of birth. A median BMI was computed for each patient
using all BMI measures listed in their files. The median BMI was
selected as a more reliable value (less susceptible to outliers) than
the most recent measure or mean, given that a number of measures were
suspected to be in error (outside the expected range and/or computed
using weight in pounds rather than kilograms). Since BMI does not
generally change a great deal over time [18],
use of a fixed BMI measure is justifiable. The concurrent health
conditions reported consist of conditions for which validated case
definitions were developed by the CPCSSN: hypertension, depression,
osteoarthritis, and chronic obstructive pulmonary disease (COPD).
Diabetes medication prescription was identified using ATC
classification. This information was categorically transformed to
approximate diabetes type and severity: insulin only (T1DM), oral
diabetes medications only (non-insulin-dependent T2DM), and both insulin
and oral diabetes medications (insulin-dependent T2DM).
Statistical analyses
The sample population is described using frequencies
and proportions, and means and standard deviations, as appropriate.
First, the characteristics of the sample of patients with diabetes and
prescribed ADs in 2014 (n=10,152), stratified by sex, are reported.
Second, AD prescription frequencies and proportions (by pharmacological
class and individual AD agent) for the 2014 cross-section, stratified by
sex and history of depression, are reported. Finally, as a sensitivity
analysis, the frequencies and proportions of AD prescriptions are
described through a 5-year comparison of annual cross-sections of
patients prescribed ADs between 2009 and 2014. Analyses were performed
using SAS version 9.4.
Ethics
The CPCSSN received ethics approval from the research
ethics boards of all host Universities for all participating networks
and from the Health Canada Research Ethics Boards. The present study
received ethics approval from the McGill University Faculty of Medicine
Institutional Research Board.
Results
Population characteristics
Table 1 provides
description of characteristics of diabetic patients prescribed ADs in
2014 (n=10,152), stratified by sex. This sample is described according
to age, BMI, presence of co-morbidities and anti-diabetic medication
prescription. In the cohort of diabetic patients prescribed ADs in 2014,
more of the patients were female than male. Among those with BMI
measurements (n=7, 387; 27.2% missing), almost all were overweight and
nearly two thirds were obese (BMI>30kg/ m2). History of
depression was identified in over half of the sample. With regard to
other comorbidities, hypertension was most frequent, followed by
osteoarthritis and COPD. Regarding prescription of anti-diabetic
medication, most were prescribed oral medications, followed by a
combination of oral medications and insulin, and less than 10% were
prescribed insulin alone. In over¼ of the diabetic patients, no
prescription of diabetes medications was identified.
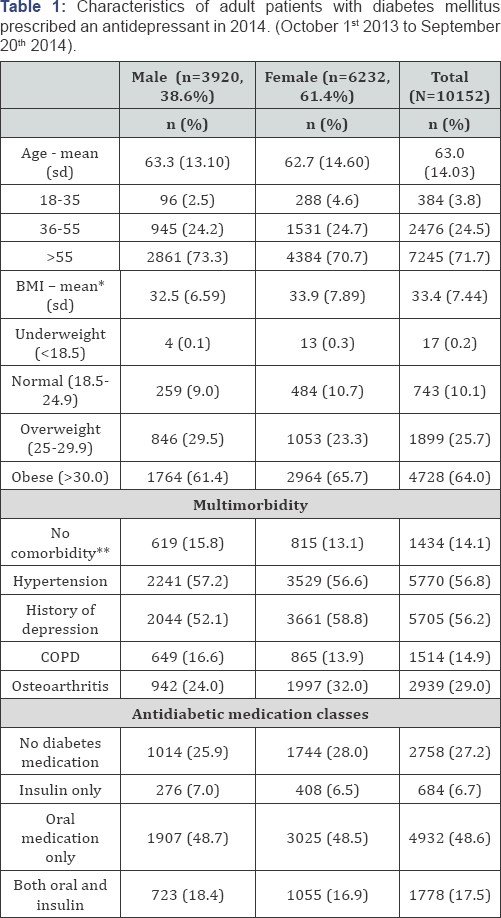
*Group mean of individuals' median BMI values
**None of the conditions for which CPCSSN case definitions were developed
Characteristics of males and females in the sample
were generally comparable, with a few exceptions. Mean age and mean BMI
(group mean of the individuals’ median values) were comparable between
the sexes. Males were only slightly older than females, and slightly
more females were obese than males. Very slight differences in diabetes
medication prescription were observed, with more males than females
prescribed insulin (either alone or in combination with oral
medications).
Antidepressant prescription
Table 2
presents the frequency and proportion of ADs prescribed for the 2014
cross-section of diabetic patients, in terms of pharmacological class
and individual medication, stratified by sex and history of depression.
The most frequently prescribed AD classes given to people with diabetes
were SSRI, followed by SNRI, TCA, SARI, NDRI, NaSSA and MAOI. A trend
was observed in which the prescription of certain ADs for patients with a
history of depression differed from those without. For diabetics with a
history of depression, the most commonly prescribed classes were SSRI,
followed by SNRI, TCA, SARI, NDRI and NaSSA. The most frequently
prescribed classes of AD given to diabetic patients without depression
were TCAs, followed by SSRIs, SNRIs, SARIs, NDRI and NaSSA.
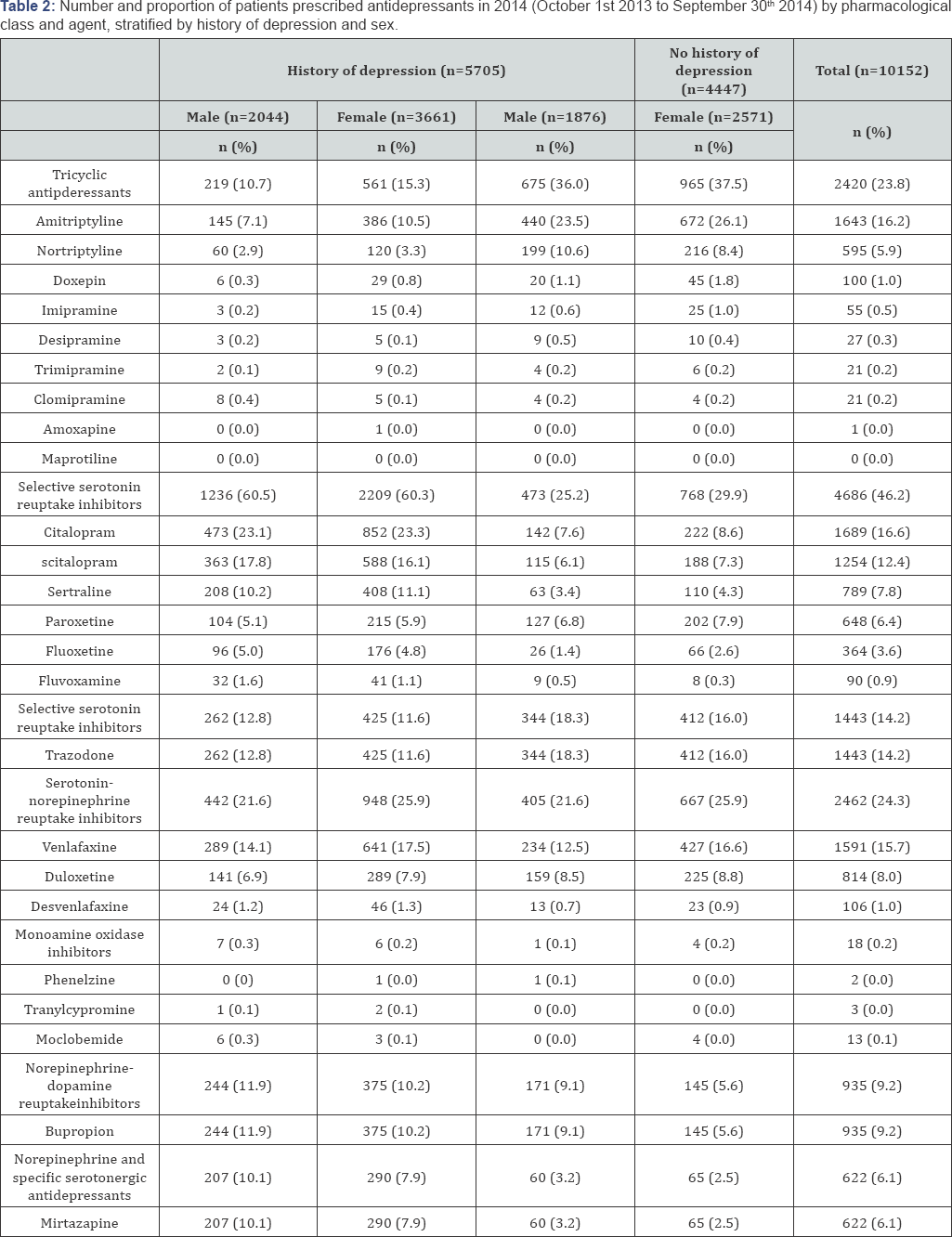
The most frequently prescribed AD agents given to
diabetic patients with a history of depression were Citalopram,
Escitalopram, Venlafaxine, Trazodone, Bupropion, Amitriptyline and
Sertraline. For diabetic patients without a history of depression, the
most frequently prescribed ADs were Amitriptyline, Trazodone,
Venlafaxine, Nortriptyline, Duloxetine, Citalopram and Bupropion. In
people with diabetes and a history of depression, more females than
males were prescribed ADs in general. The proportion with which
individual ADs were prescribed were generally comparable between the
sexes, with a few exceptions. Amitriptyline and Venlafaxine were more
often prescribed for females than males, and Mirtazapine was more often
prescribed for males than females.
For diabetic patients without a history of
depression, larger differences were observed. The prescription frequency
was higher for females than males for each of the individual SSRIs;
Amitriptyline, Nortriptyline and Venlafaxine were more frequently
prescribed for females than males; and Bupropion was more prescribed for
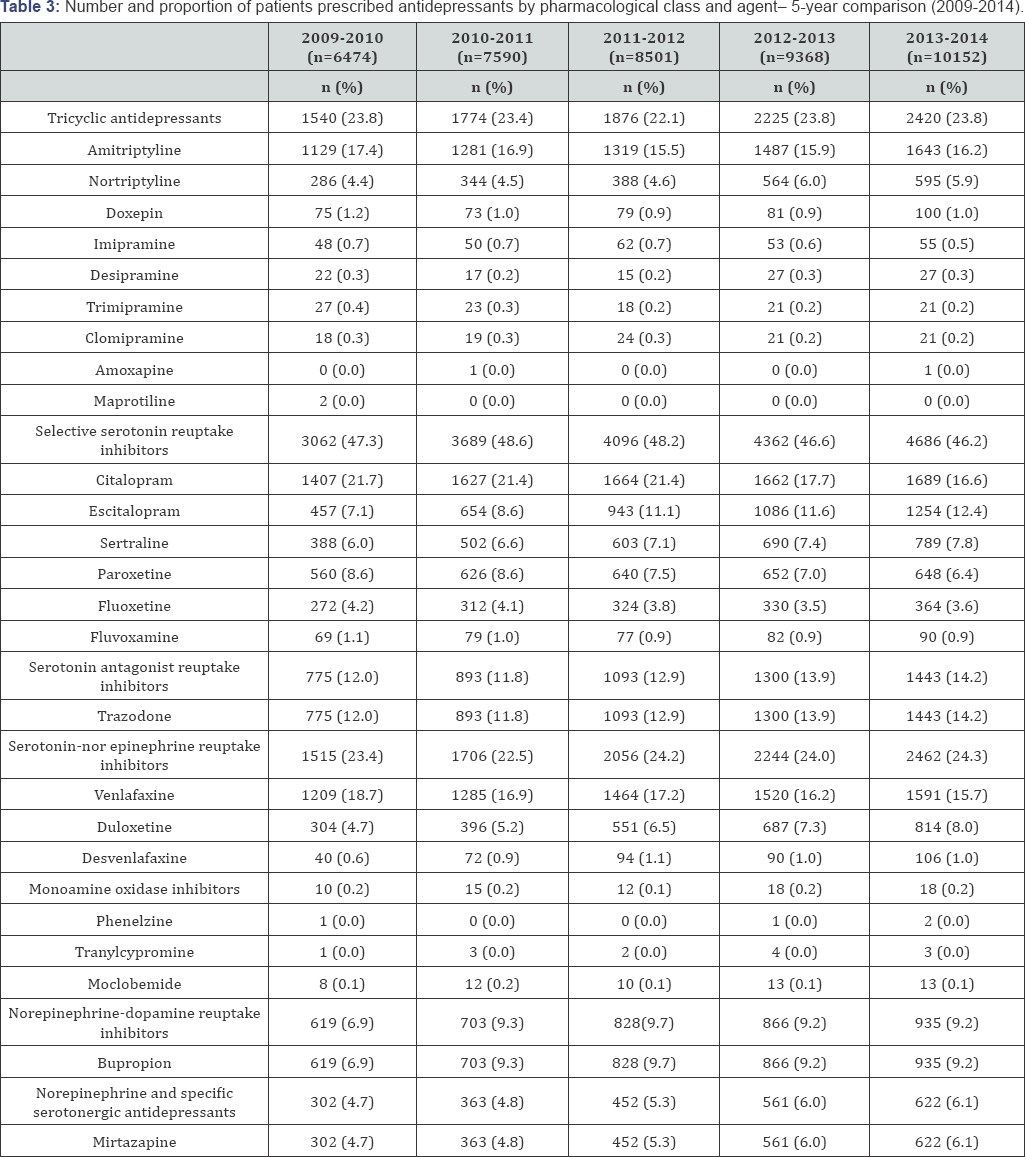
males than females. Table 3
provides a comparison of 5 annual cross-sections of diabetic patients
prescribed ADs between 2009 and 2014. Across the 5-year span, the
relative proportions with which the pharmacological classes were
prescribed remained stable. Changes in proportions were observed for
individual medications within the classes, however. Increases in
relative prescription frequency was observed for Escitalopram,
Duloxetine, Bupropion, Mirtazapine and Trazodone. A decrease was
observed for Citalopram, Paroxetine, Venlafaxine and Amitriptyline.
Discussion
Interpretation
The present study provides a description of AD
prescription in Canada for people with diabetes. This appears to be the
first epidemiological study of primary care practices describing the
prescription of ADs for people with diabetes in Canada. Additionally,
very few studies to date have described the prescription of ADs in terms
of individual medication.
This study's findings regarding the proportion with
which the different classes of ADs were prescribed for people with
diabetes and a history of depression are consistent with other research
using CPCSSN data but described the prescription of ADs in a Canadian
primary care population with a history of depression (with and without
diabetes) [12].
The finding that SSRIs are most frequently prescribed class of AD is
consistent with literature suggesting SSRIs are the standard of care for
depression [19]. Evidence from clinical trials suggests SSRIs and NDRIs may be associated with improved glucose metabolism [7,20,21] and that TCAs and SNRIs may be associated with impaired glucose metabolism [8-10].
The mechanisms explaining these findings are inconclusive, but research
suggests that the ADs binding profiles (the transporter and receptor
affinity) play an important role [13,22,23].
The present study shows that almost half of diabetics prescribed ADs
were given SNRIs or TCAs. While evidence so far is inconclusive, the
frequency with which these ADs are prescribed may be cause for concern
as it appears that primary healthcare providers are not aware of the
negative impact of these medications with regard to glucose metabolism.
Given the similarity in prescription patterns for the general primary
care population with a history of depression [12]
and diabetic patients with a history of depression, it appears that
health care providers’ AD prescription choices are not affected by
current evidence regarding the risks certain ADs pose for people with
diabetes.
This study found that over half of the diabetic
patients prescribed ADs had a history of depression. History of
depression was used to define those for whom ADs were prescribed for the
treatment of depression. The prescription of ADs for people with
depression tended to differ from those without. This is to be expected
as ADs are prescribed for a number of other conditions than depression,
including: general anxiety or panic disorders, obsessive-compulsive
disorder, and eating disorders; and clinically accepted off-label
indications include insomnia, tobacco-cessation, headaches, neuropathic
pain and chronic pain [24].
In patients without a history of depression (and those with a history
of depression but were prescribed an AD for the treatment of another
condition), the ADs were more likely prescribed for other conditions.
The trend of differing prescription frequencies between males and
females for specific ADs is largely related to the frequency with which
these conditions are presented and treated in primary care.
Between 2009 and 2014, an increase in AD prescription
frequency was observed; however, this may be a reflection of gradual
increases participating clinics as well as their data capture. Increases
in relative prescription frequency were observed for Trazodone,
Bupropion and Mirtazapine, for which little research on their effect on
glycemic control has been published. Citalopram and Paroxetine (SSRIs)
decreased in frequency, while Escitalopram, an alternate SSRI,
increased; and Duloxetine (SNRI) decreased while Venlafaxine, an
alternate SNRI, increased. A slight decrease in prescription frequency
was observed for Amitriptyline (TCA), relative to an increase in the
prescription of Nortriptyline, an alternate TCA. Despite growing
evidence that TCAs are associated with impaired glucose metabolism [7,8,25,26] no change in proportional frequency was observed over the course of the five-year observation period.
Limitations
One limitation is that the sample is only somewhat
representative ofthe general Canadian population. In comparison with
2011 Canadian census data, the CPCSSN population in 2013
over-represented older adults and under-represented younger adults; and
the CPCSSN population comprised significantly fewer young adult males
than the general Canadian population [27].
Furthermore, given that the practices participating in the CPCSSN were
not randomly selected, the population may not be generalizable to the
Canadian primary care population [27].
Participating practices tended to be those affiliated with the
practice-based research networks involved in the project and those more
engaged in chronic disease surveillance. Nevertheless, the trends
observed with this sample are expected to compare to those in a wider
population. Future research should seek to confirm this hypothesis.
Second, the case detection algorithms for depression
has a relatively high false positive rate. The case definition for
depression detects lifetime depression, and includes manic disorders and
bipolar mood disorders. Lifetime depression was used in this study to
approximate the prescription of ADs for the treatment of depression as
AD dose and reason for prescription were not consistently recorded or
could not be coded. Patients with a history of depression may be given
ADs for other conditions. For instance, TCAs are more commonly
prescribed insomnia and chronic pain, Mirtazapine is more commonly
prescribed for smoking cessation and Trazodone is more often prescribed
in low doses as a hypnotic [28,29].
Given the number of ADs prescribed to people with depression, use of
lifetime depression as an approximation over-estimates the number of ADs
prescribed for the treatment of depression.
A third limitation of this study pertains to the use
of health records for research. While primary care EMRs permit the
naturalistic examination of prescriptions and health conditions over
time, some values may be missing (not entered or could not be coded) and
some fields may differ between EMR products or may not be used in a
standardized manner by primary health care providers. Were the data
available, AD dose, refer to psychotherapy and diagnoses for other
health conditions for which ADs are prescribed would have been included
to better describe depression treatment practices in primary care
patients living with diabetes.
Conclusion
The present research study provides information on
the prescription of ADs for people with diabetes in primary care
practices. This information is valuable as it provides insight into the
implications of research evaluating the impact of ADs on glycemic
control in people with diabetes. As new and more conclusive evidence on
the effects of ADs on blood sugar emerges, or as new clinical
recommendations are introduced, this study provides the means of
estimating the number of patients that will be affected.
Acknowledgement
JG received a travel award for this research from the
Canadian Institutes for Health Research (CIHR) and a travel award from
the McGill University Department of Family Medicine. SSD is
Chercheur-BoursierClinicien, supported by a Fonds de Recherche Quebec
Sante award. This research was part of the CPCSSN initiative, which is
funded by the Public Health Agency of Canada (PHAC) under a contribution
agreement with the College of Family Physicians of Canada on behalf of 9
practice- based research networks associated with departments of family
medicine across Canada. The views expressed herein do not necessarily
represent the views of the PHAC.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
https://juniperpublishers.com/crdoj/index.php


Comments
Post a Comment