How Misconception of Insulin Therapy Affects Type 2 Diabetes Mellitus Patients' Acceptance on Daily Injection
Authored by FU Sau-Nga
Abstract
Objectives: To find out the development of
misconception that leads to Psychological Insulin Resistance in type 2
diabetes mellitus patients.
Methods: 24 focus group interviewsof124insulin
naive Chinese patients in 11 primary care clinics. Thematic analysis of
the interview transcript was based on patient's expectation of insulin
injection in their physical, psychological and social view, to identify
the origin of negative attitudes.
Results: Three main sources of misconception
are: 1) lacking adequate knowledge, 2) conflicting medical advice, and
3) hearsay from community. Most participants never saw the insulin pen.
Patients deferred insulin commencement because they could choose among
different clinicians' medical advice. Patients commonly keep peace of
mind rather than trying daily injection. They took daily injection as a
stigma and ignored the possible DM complications.
Conclusion: Different parties contributed to
the development of misconception on insulin therapy. Clinicians should
identify and control patients' possible misconceptions.
Introduction
Type 2 diabetes mellitus (T2DM) is increasingly
prevalent worldwide. In order to reduce complications, insulin
replacement therapy is frequently required because of the progressive
nature of T2DM [1]. However, patient refusal of insulin is often found [2] as a result of psychological insulin resistance (PIR), which means a strong negative attitude against insulin therapy [3]. When comparing to the western countries (28% [4]), the prevalence of PIR has been particularly high in Asia (70.6% [5]).
PIR involves such a wide range of adverse emotions and practical
concerns as questioning the necessity to intensifying medication by
insulin, pain, phobia, failure, fear of side effects, operation of
insulin pen, economic cost for insulin therapy, language barrier,
inadequate knowledge, poor social support, perceived damages on personal
image, social life and perceived clinicians' negative attitude towards
insulin [4]. In line with the higher PIR in some ethnic groups, it was well-documented that female [5], people with lower income, lower educational level [6], older age group [7], lower glycoslated haemoglobin (HbA1c) level [8], being insulin naive [9] were more unwilling to commence insulin.
Clinicians have tackled PIR as a complex and
multifactorial phenomenon by patient-centered approach and through the
recommended clinical practices. Most countries including Hong Kong have
at the same time adopted newer insulin delivery devices, commonly
insulin pen, with shorter and thinner needle that enables injection ease
and reduces pain. It is therefore pressing to examine why PIR still
commonly circulates among T2DM patients, especially those relatively
older, with lower income and lower educational level. This study adopts a
qualitative research approach to take a close scrutiny of how patients
acquired different knowledge about insulin therapy, and why negative
perceptions and emotions are resulted from this knowledge [10].
The findings from this study advance insights for formulating proactive
strategies that may possibly enhance the acceptance rate of insulin
injection.
Methods
Setting
The study sites were eleven government-funded primary
care clinics, where provide health care for more than 25,000 people
with T2DM in urban Hong Kong annually. The majority of the visiting
patients are older Chinese, relatively less educated, and from the lower
social economic class [11].
The consultation fee for each visit is USD6. All prescriptions and
investigations are free of charge. Some patients not only consult the
clinicians in public setting, but also pay out of their own pockets to
attend
Since 2009, some ofthe public primary care clinics
have provided insulin commencement for indicated T2DM patients.
Free-of-charge injection pen and vials of insulin are provided. Patients
only need to pay for the needles of injection pen and the consumables
for self-glucose monitoring. However, the successful cases of commencing
insulin remain a few. From 2010 to 2012, only less than 4% of patients
with T2DM had successfully started on insulin therapy [11].
Participants
This study included insulin naive T2DM patients on
maximum tolerated dose of oral antidiabetic agents (OAAs). Their latest
haemoglobin A1c level was ≥7.5% (58.5 mmol/mol). Subjects under
18-year-oldor being pregnant were excluded.
Study design
The moderators conducted focus group interview by
asking broad views from participants about insulin therapy, before
asking focal questions on the development of misconceptions identified.
Focus groups were used in order to collect group interaction that
encourages participants to explore and clarify attitudes, priorities,
group norm and cultural value [10]. All participants offered their written informed consent.
The interviews were conducted in clinic meeting rooms
from June 2013 to May 2014. Each focus group interview ran with 3 to 8
participants and lasted for 60 to 90 minutes. One moderator (one of the
authors) and one observer (research assistants) were arranged to conduct
the focus group interview in Cantonese (one of the Chinese
language)according to thestandard interview protocol. (Supplementary
Data S1)Investigators avoided interviewing our own patients. The focus
groups interviews were terminated when data saturation was reached after
24 focus groups,where adding participants to the existing sampleis
unlikely to generate any new ideas [10].
Data analysis
All focus group interviews were recorded as digital
audio files and transcribed verbatim into Chinese. The transcript was
entered into NVIVO 10® (QSR international) in Chinese for data analysis.
A coding tree with definition and operational guidelines for each code
was formulated. The authors employed thematic analysisto identify
important themes, patterns, features, meanings as well as issues and
stories. Finally, SF translated the selected data into English. SC then
translated the transcript back into Chinese to assess translational
equivalence. Discrepancies between the original Chinese items and
back-translated items were reviewed and modified by allauthors.
Results
Characteristics of participants (Table 1)
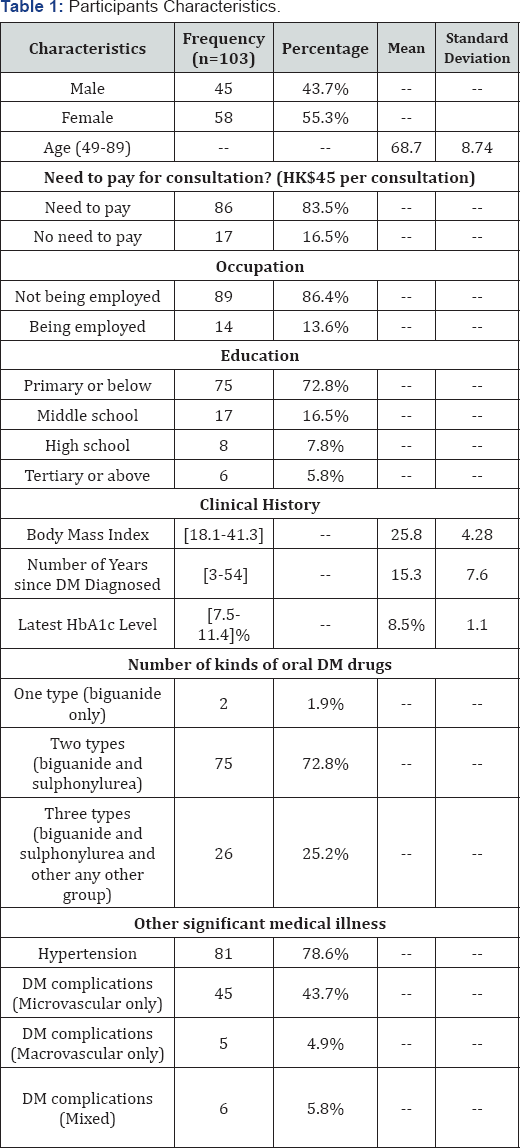
Note: DM: Diabetes Mellitus
* Reasons of �no need to pay�includes being staffs or dependents of government or hospital authority, on social security scheme.
**Not being employed includes being housewife, retired, or unemployed.
***DM complications includes any microvascular or macrovascular complications related to DM
124 participants (mean age= 68.1, M:F ratio = 1.03)
were interviewed in 24 focus groups. Most participants (86.3%) were not
in full time employment (i.e. housewife, unemployed or retired). Their
educational level was relatively low: 67% attained primary school
education or below, while only 5% received tertiary education. Their
mean latest HbA1c amounted 8.5% (69.4 mmol/mol) and that indicated poor
glycaemic control. The majority (98.4%) were prescribed with two or more
types of OAAs.
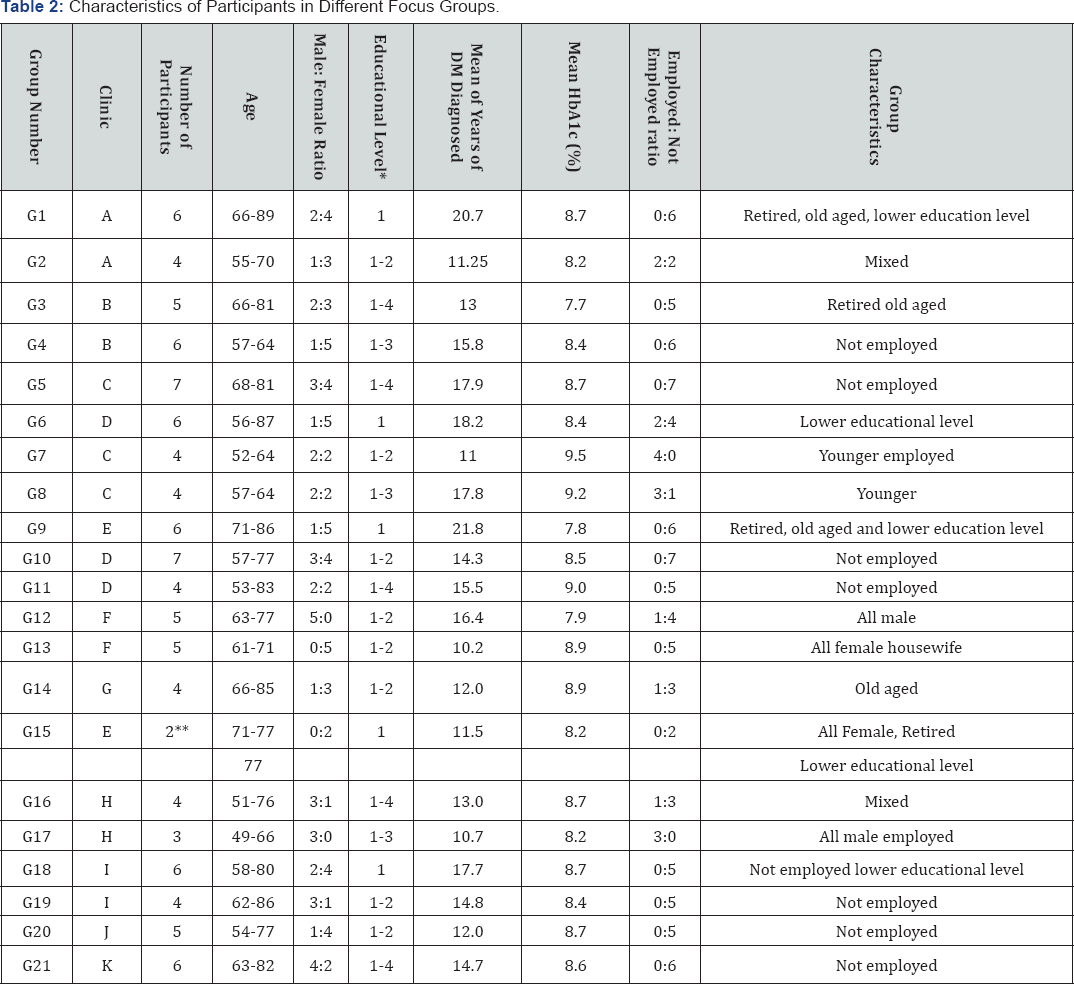
* 1 = primary or below; 2= middle school; 3 = high school; 4 = university or above
Major findings
The characteristic of different groups were shown in Table 2.
Misconception in this study refers to any inaccurate idea, belief,
myth, presumption and conjecture that deviate from the proven medical
knowledge. The three main sources of misconception among the
participants are: 1) lacking adequate knowledge 2) conflicting medical
advice, and 3) hearsay from community. All participants' names were
replaced by assigned number P1, P2, P3, etc. Group names were assigned
as G1 (Group 1), G2,etc.
Misconceptions from lacking adequate knowledge (Table 3)
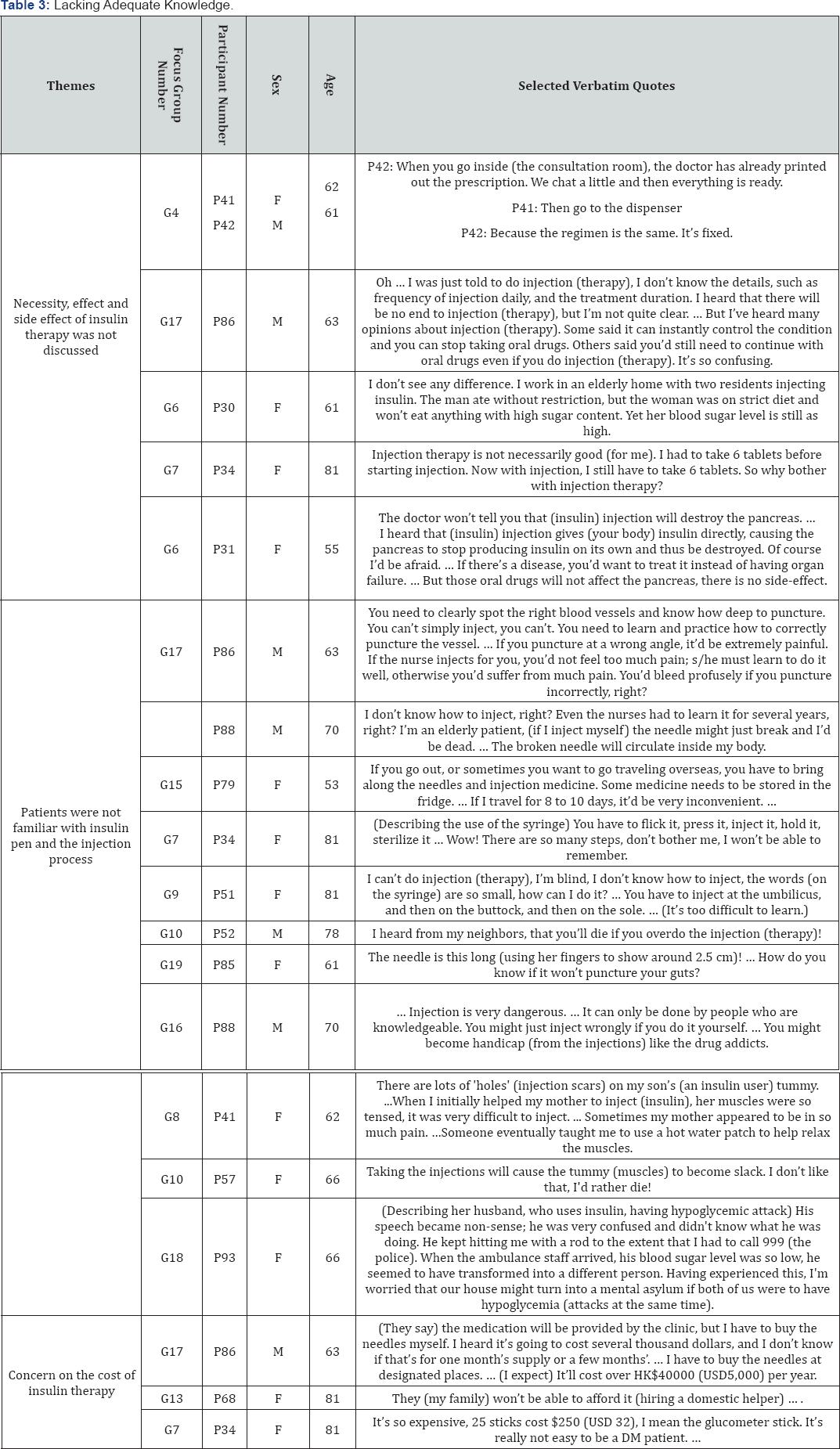
Most participants confirmed heavy psychological
burden such as fear, anxious, shock, depressed if they had to commence
insulin as most of literature description [4]. Almost all participants did not know or could not give accurate information about insulin pen or injection process.
Necessity, effect and side effect of insulin therapy was not discussed:
The discussion between P41 (female, 62-year- old) and P42 (male,
61-year-old) in G4 described an extreme situation of the communication
with doctors. Doctors would print out prescription sheet few minutes
after consultation started. The patients therefore felt that there was
no need to understand insulin therapy. Others participants reported that
they would strongly challenge their doctors about the necessity of
using insulin therapy. While they recognized that the effect the
effectiveness of insulin therapy, particularly what was its of oral drug
would be diminishing, they had no idea about difference fromoral drugs
in controlling blood sugar.
Likewise, discussion of the side effects of insulin
was insufficient. Three participants P31 (female, 55-year-old), P75
(male, 70-year-old) and P88 (male, 73-year-old), from 3 focus groups
expressed a shared worry that exogenous insulin would take over
remaining pancreatic function and thereby result in organ (pancreas)
failure. They suspected direct injection of insulin was overly potent.
It would therefore stop pancreatic cells from producing insulin. Other
commonly exaggerated insulin side effects include chronic neuralgic
pain, profuse bleeding, broken needle, punctured internal organ and
consequential scars over body with many holes, and subsequent changes of
skin texture and colour. Air bubbles might be injected into body that
could result in death. Few participants described their observation of
hypoglycemic attack of their relatives. The victim became
uncontrollable, insane and unable to handle. Collectively, insulin
injection should be avoided at all cost for self-preservation.
Patients were not familiar with insulin pen and the injection process: On the contrary to the existing research finding that most insulin naive DM patients were familiar with insulin pen [12],
most participants in this study never sawan insulin pen, much less the
injecting process. Consequently,some participants associated injection
of insulin with what they saw and felt in their existing experience from
their visits to clinics or hospitals. The needle is a much longer and
bigger, 20 or 25 -gauges and 25 to 30 mm long. This explained why some
participants were prompted into anxiety, fear of pain, phobia of blood,
and other physiological responses (e.g., chills, rigor, sweating and
palpitation).
Participants generally perceived that the injection
of insulin was a complicated process requiring intensive professional
knowledge and training. The storage of insulin, the sterilization of
instruments, and the steps for injecting were all highly demanding and
rigorous. Some participants illustrated the difficulty of injection by
their clinicians' multiple attempts before successful venepuncture even
though they were professionally trained. Injection of insulin was
definitely beyond their literacy, knowledge and ability to handle.
Various sites for insulin injection were also aired amongst the
participants such as buttock, cubital fossa, umbilicus, anus and even
the sole. It bothered much more the older age group because of their
illiteracy in English, some also in Chinese, and their decline in
eyesight and hand functioning.
Concern on the cost of insulin therapy: Given
that most participants came from the lower socio-economic class, they
worried much about the cost of insulin therapy. Some participants
thought that they had to buy the pen and injection medicine from their
pocket. In fact, people on insulin therapy only need to buy the needles
of insulin pen that costs HK$200 (USD25) per month. The cost would be
reimbursable if they were on the social security scheme. However, nearly
none of the participants were clear about the policy. P86 (male,
63-year- old) even estimated the regular expenses for insulin therapy to
be up to HK$40,000 (USD 5,000) per year. In line with the drug cost,
P68 (female, 81-year-old, lives alone) worried about the additional
financial cost for employing a helper to perform injection for her.
Misconceptions from conflicting medical advice (Table 4)
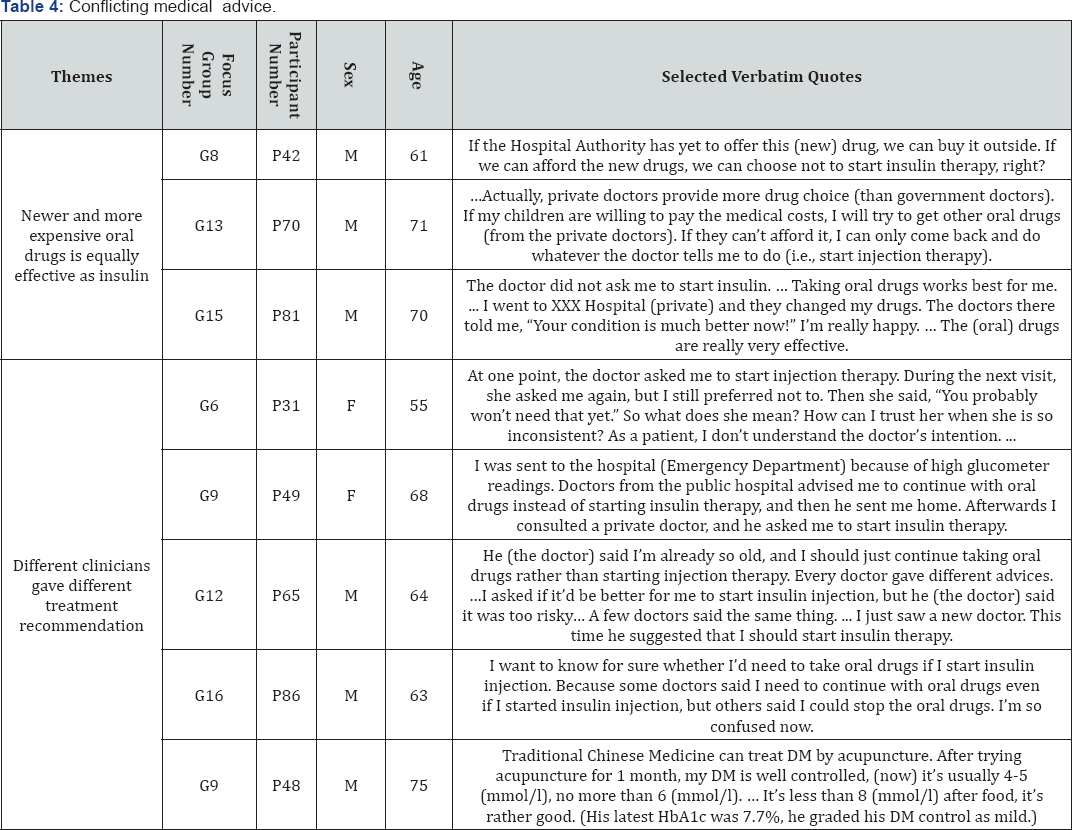
Most participants reported that the continuity of
care from public and private doctors for their chronic illnesses was
generally poor and the consultation time was short and erratic. If
different clinicians gave different opinions, it confused patients of
which DM treatment was the best in their condition. As a result, most
participants simply chose the advice that supported their intention to
delay or avoid insulin therapy.
Newer and more expensive oral drugs is equally effective as insulin:
Many participants believed newer generation of OAAs that was ever
effective and potent in controlling their blood sugar. The switch to
insulin therapy was therefore deferrable if one could afford the
expensive newer generation of OAAs. P58 (female, 55-year-old) claimed
that she regularly attended both public clinics and a private doctor.
While her latest HbA1c had been already up to 10.7% (93.4mmol/mol), she
appreciated her private doctor who reassured and prescribed her with
"drugs not available in public clinics". She adhered to oral therapy and
had no intention to start insulin therapy. Such form of personal
presumption gives rise to a myth in real life: the deferability of
insulin therapy depended on money.
Different clinicians gave different treatment recommendation:
The most common advices from clinicians were "you should be more
careful about what you eat", "you should get out and move about" when
the participants' blood sugar was high. They have an impression that
one's success or failure in maintaining the optimal blood sugar level
was solely a matter of diet and lifestyle control. P65 (64-year-old)
knew that his blood sugar was always high, which was harmful to his
health. He was hesitated whether he should start insulin therapy or not.
Some doctors encouraged him, but one of them told him that he was too
old, and therefore too risky to start insulin therapy. Overall, our
participants commonly perceived clinician's negative attitude towards
insulin.
Misconception from Hearsay from Community (Table 5)
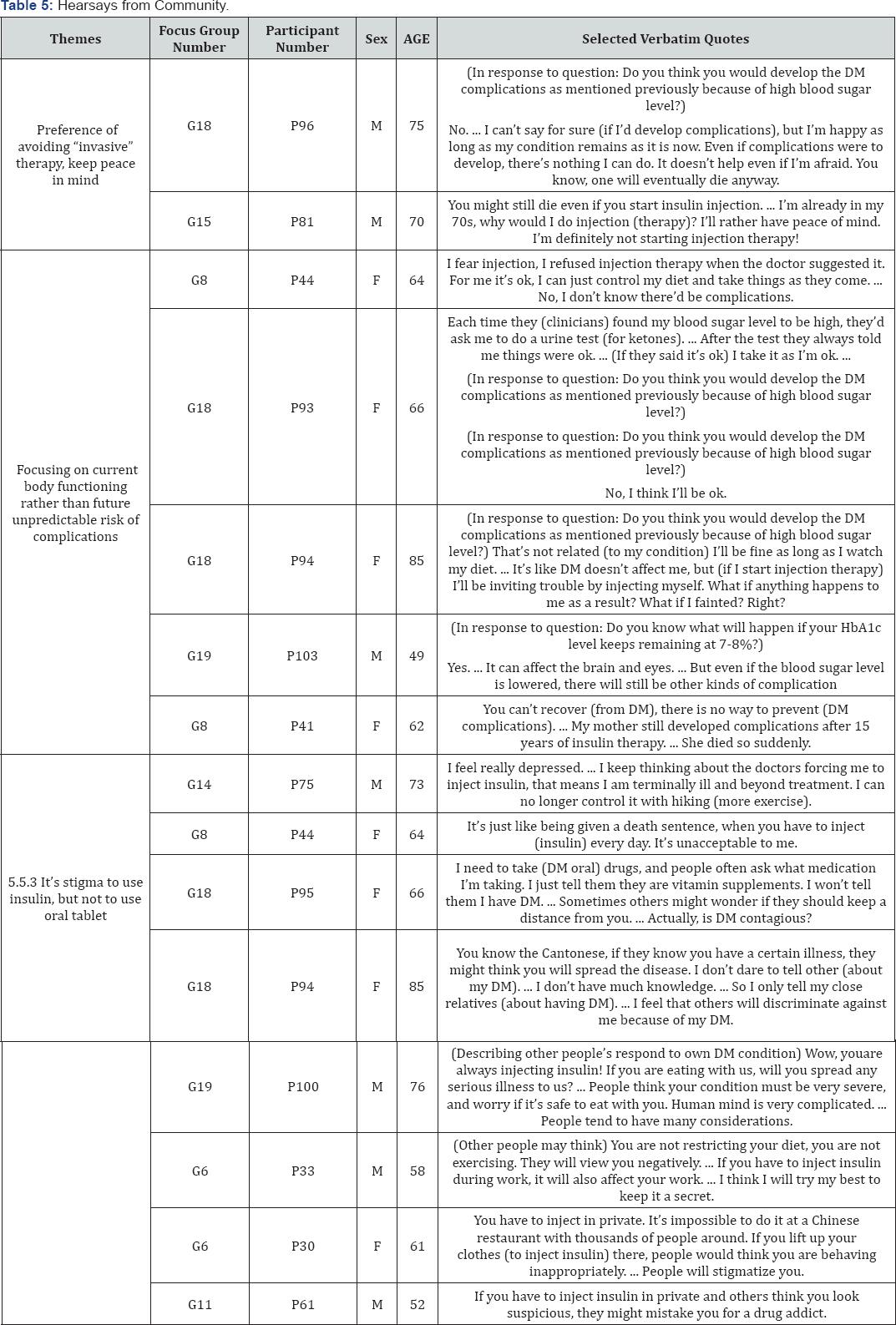
Discussions from focus groups showed that most
participants were haunted by the rumours and myths from one's social
circle and from the media such as newspaper and online discussions.
Preference of avoiding “invasive” therapy, keep peace in mind:
The older participants often expressed their will of keeping peace in
their remaining life because their age is approaching the end. Any
procedure or treatment that would increase physical suffering should be
avoided. They preferred minimal use of drugs in any form. They believe
that self-injection could not improve their health but only add
suffering. Some of the participants even regarded daily injection
as"torturing their remaining life.
Focusing on Current Body Functioningrather than Future Unpredictable Risk of complications:
In order to justify their resistance to insulin injection, many older
participants cited the hearsay from community that the rise of DM
complications was independent of the blood sugar control. Most of them
at the same time denied their risk of having complications because they
had been well-disciplined in diet control and regular exercising. They
did not experience any disabilities or ill-health sensation at the
moment. They would emphasize current situation and would not bother
"future risks".
It's a stigma to use insulin, but not to use oral tablet:
Most participants favoured the oral therapy largely due to their
concern on self-dignity and social status. Some of them would like to
cover up their condition of having DM. Others did not mind being known
the need of regular oral drug-taking always because it was generally
acceptable in the community. Even when others saw them taking oral
tablets, P95 (female, 66-year- old) said that she could simply liethat
she was taking vitamin supplement when she was questioned.
Similar to other research finding, the use of insulin in the Chinese peoples' view represented a person to be really sick [13],
P44 (female, 64-year-old)expressed that she would feel like "being
given a death sentence" if she had to inject insulin every day. P75
(male, 73-year-old) from G14 claimed that he would be depressed if he
had to commence insulin. He used to reduce his blood sugar by increasing
the amount of physical activities. Failure to reduce blood sugar by his
own effort meant that he lost control of his own body. Other
participants also associated insulin users with some negative images
such as the drug addict. The association was not only their personal
imagination but also a common sense in the community. They thus found it
egregiously stigmatizing if others knew that their body functions
relied on daily injections. The comment from P100 (male, 76-year-old)was
illustrative: "people would look down on you if they know you are using
needles. ... They probably think that you have a contagious disease!"
This was particularly troubling to participants who were employed, such
as P62 (male, 58-year- old). Their main concern was that if their
colleagues saw their daily insulin injection, they might be viewed as a
"weak," a "handicapped," or a "criminal." Consequently, they might lose
their job.
Discussion and Conclusion
Discussion
This is the first study in Hong Kong that adopts a
qualitative approach to investigate insulin naiveT2DM patients'
misconception on insulin therapy. The participants' socioeconomic
background were characterised mostly by not being employed,with lower
educational level and lower income. They were comparable with patients
generally found in government funded primary care clinics in Hong Kong [14].
The analysis confirms with the existing research insights to the
prevalence of PIR, particularly the lack of adequate knowledge on
necessity [15],
expected effect an dungrounded side effect of insulin therapy as
profuse bleeding, severe skin reactions, injection process, patients'
concern on treatment cost, stigmatization associated, patients' attitude
of preference to oral tablet [16], and the concerning quality of health at the moment, but not future risk of complications [17] from most of the participants.
This study advances several new insights into
patients' lived experience of how and why they became poorly informed
about the treatment options. There were multiple sources from daily
knowledge to social network. First of all, the DM patients in this study
were not familiar with the insulin pen as the DM patients from other
countries [12].
Many patients in Hong Kong primary care setting have never seen the
insulin pen, much less understanding of the injection process. Under
consultation time constraint, there were few opportunities for
discussion about insulin therapy in either causal or structural
manner.The result of poor patient-clinician communication was that many
patients would favour and accept hear says. Some would even believe that
exogenous insulin was toxic to pancreatic cells, and speeded up organ
failure.
This study also found that the presence of
conflicting medical advice opened the rooms for patients to run upon
their preference for treatment. Without a consistent medical advice for
the switch to insulin therapy, patients occurred to distort what the
clinicians suggested them to do for their health in various manners. For
instance, when doctors suggested newer generations of OAAs and insulin
as options of managing hyperglycemia, patients might interpret the newer
drugs as replacement of insulin therapy. While clinicians advised
patients to maintain a proper diet and lifestyle, patients might believe
that the blood sugar can be largely controlled by that alone.
Clinicians should be alert to such over-interpretations and the like by
clarifying the details and giving the sufficient information for
patients. Another important finding from this study appears to be the
presence of a remarkable difference between the Western and the Chinese
DM patients. Namely, the Chinese patients concerns less on fear of
weight gain and hypoglycaemia as the Western patients did [18].
In line with their negative evaluation of insulin therapy, the Chinese
patients instead concern more on keeping peace in mind. They avoid being
stigmatized as a sick person while they consider insulin commencement [19].
They also appealed to hear says from community to justify their
indifference to DM complications and resistance to insulin therapy.
Clinicians should aware of patients' attitude on stepping up drugs,
especially in relatively older patient in order to arrive share
understanding of disease management [20].
Conclusion
This qualitative study demonstrates how the
prevalence of PIR involves misconceptions on insulin therapy among
people with T2DM and in the general public. The three major sources of
misconception include the lack of adequate knowledge, conflicting
medical advice, and hearsay from community. When T2DM patients failed to
rectify them is conceptions, their selfefficacy in starting insulin
therapy will be undermined as what the research subjects in this study
indicated. The possible improvement of the acceptance rate of insulin
therapy from the improvement of insulin delivery devices will be equally
upset due to the continuation of a large gap of the T2DM patients from
what are the proper medical understanding and doings. Clinicians should
be therefore sensitive to the rise of such misconceptionsin part of
their actions to ensure the offering of proper insulin therapy forT2DM
patients.
Acknowledgement
The study was funded by the
Health and Medical Research Fund, Research Fund Secretariat, The Food
and Health Bureau, the government of Hong Kong Special Administrative
Region (grant number: 11122751, URL: https://rfs2.fhb.gov.hk/app/
fundedsearch/projectdetail.xhtml?id=1386 ).
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
https://juniperpublishers.com/crdoj/index.php


Comments
Post a Comment