Screening For Cushing's Syndrome in Primary Care: Which Test is The Best?
Introduction
Cushing's syndrome (CS) is defined as an outcome of
prolonged exposure to glucocorticoids whether from outside or inside
sources. It's a relatively rare condition with an incidence of 0.7-2.4
per million population per year [1]. Clinical presentation in primary
care setting can be highly variable, and establishing the diagnosis can
often be difficult and is frequently missed due to its rarity and
overlapping characteristics with common disorders like metabolic
syndrome. Early diagnosis and treatment of CS is associated with a
decrease in morbidity and mortality [2]. The objective of this article
is to discuss the most appropriate screening test that could be
performed in primary care in clinically suspected cases of CS.
Etiology of Cushing’s Syndrome
Exogenous administration of glucocorticoids
(Iatrogenic CS) is the most common cause of CS. Table 1 shows the
various causes of endogenous CS. ACTH dependent CS accounts for 80-85%
of cases, of which around 75-80% are due to pituitary adenoma. Chronic
alcoholism, depression and severe obesity may lead to reversible
hyperactivity of HPA axis and cause pseudo-CS [1,2].

Clinical Features of Cs
Table 2 discusses the various clinical features of
CS. Certain features of the skin, muscles and bones are specific for CS
that helps to differentiate it from simple obesity. Clinical features
like cataract, raised intraocular pressure, aseptic necrosis of femoral
head and osteoporosis are more common in iatrogenic CS [1].

Whom to Screen
Although CS is relatively rare, studies of patients
with diabetes, obesity, hypertension, and osteoporosis found a high
prevalence of CS among these populations [3]. The Endocrine Society
guidelines recommend screening under the following circumstances: [4]
• Patients with multiple, progressive, and discriminatory findings suggestive of CS.
• Cases with unusual features like hypertension or osteoporosis at a young age
• Children with a decreasing height percentile and increasing weight
• Adrenal incidentalomas
• Patients with familial disease that puts them at risk of CS.
• It recommends against widespread testing for CS other than the above patient group.
Screening Tests for Cushing’s Syndrome in Primary Care Settings (Table 3)
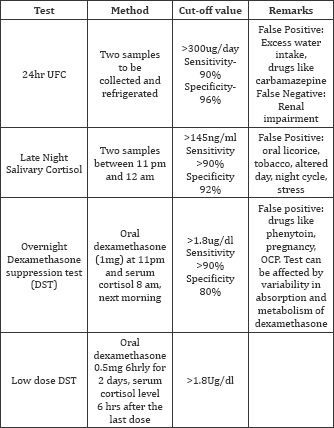
It is recommended by the Endocrine Society guidelines [4] that one of the following tests be performed for screening of CS:
1. 24hr Urinary free cortisol (UFC) (at least two measurements)
2. Late-night salivary cortisol (two measurements)
3. 1-mg overnight Dexamethasone Suppression Test (DST)
4. Longer low-dose DST (2mg/d for 48h)
24hr UFC
24 hr UFC looks at the unbound cortisol secretion
that is filtered by the kidneys over a 24hr period and is not affected
by conditions and medications that alter Cortisol Binding Globulin
(CBG). Normal values: <90 microgram/24hours (250nmol/ day). Values
more than 300microgram/day (830nmol/day) are considered diagnostic.
Sensitivity of this test in detecting cortisol excess is 95%,
specificity is 98%. False positive and false negative results may occur
(Table 3). UFC should be confirmed with repeat testing [5].
Late night salivary cortisol
Physiological cortisol secretion follows a circadian
rhythm. Serum cortisol concentration reaches its peak in the morning
(0600-0800h) and is lowest in the night during the first half of normal
sleep. Normal circadian rhythm of cortisol secretion is lost in patients
with CS. Salivary cortisol is measured at 23:00 hours and 07:00 hours
using a standard cortisol radioimmunoassay (RIA). The upper limit of
reference range is 145ng/dl (3.6nmol/L) and sensitivity is >92%. LNSF
is a simple and reliable screening test for spontaneous Cushing's
Syndrome and useful for screening large, high risk population (patients
with diabetes mellitus) [4].
Dexamethasone suppression test (DST)
In standard DST patient is given 1mg dexamethasone
orally at 11pm and the plasma cortisol level is measured at 8 am next
morning. In the 48-h low dose DST test, dexamethasone is given at the
dose of 0.5 mg every 6 h for 2 days at 090h, 1500h, 2100h, and 0300h
with measurements of cortisol in serum 6 hours after the last dose of
dexamethasone (normal<1.8ug/dl). The sensitivity of this test is 98%;
specificity is 80%. Normal findings in both the test make CS unlikely.
Obesity, chronic illness, chronic alcoholism and depression can cause
false positive results (pseudo-Cushing syndrome) [5].
Discussion
Cushing's syndrome is a relatively rare condition
[6], and can present to primary care in many different ways, making the
diagnosis a challenging one to reach. It is an important diagnosis to
consider, as it has a significant impact upon morbidity and mortality,
and early detection and treatment can have a significant impact on
improving life expectancy [7]. Unfortunately, however, it is a diagnosis
that is frequently 'missed', with a mean time to diagnosis of 6 years
in one study [8].
In the primary care setting, the ideal first-line
screening test would be very sensitive (ie. all those with Cushing's
syndrome would be detected, and none would be missed), practically
possible in the community, acceptable to the patient and cost- effective
[6].
Around the world all other tests except 24hr UFC,
need to be performed in the hospital setting so the most readily
available in the primary care setting is the 24hr UF [9]. 24hr UFC looks
at the unbound cortisol secretion that is filtered by the kidneys over a
24hr period. This test is usually considered overall to have a high
diagnostic sensitivity in adults and children, it is important to
correlate test results with creatinine ratios to ensure a complete
collection [4]. This test also has multiple external factors that can
cause or mask false negative/positive results such as excess fluid
intake, certain medications and improper collections. It is vital to
obtain a thorough assessment to take place to accurately access results.
[3]. In the pediatric population, even with a high sensitivity of 89%
it is still recommended to follow up the UFC with a second test
mentioned above to confirm a diagnosis [10].
24 hour urinary free cortisol levels appears to be
the most practical first-line test to perform in primary care in
patients where there is a high probability of Cushing's Syndrome,
because it is non-invasive and widely available [8]. However, in
patients who have a lower probability of Cushing's syndrome, it may be
advantageous to consider late night salivary cortisol or 1-mg overnight
dexamethasone, because both of these tests are more sensitive, reducing
the likelihood of false negative results [8]. Unfortunately, late night
salivary cortisol is not a test that is widely available to primary care
physicians in the UK [11]. The 1mg overnight dexamethasone suppression
test is possible to organize in primary care, with a well motivated
patient, but the practicalities of timing the administration of the drug
and the blood test, make it slightly more of a challenge [12].
Conclusion
In summary, when screening for Cushing’s syndrome in
primary care in the UK, a 24hour urinary free cortisol level is a useful
test for the majority of patients, particularly when they have symptoms
that make the diagnosis of Cushing’s Syndrome likely. In a patient who
is less likely to have Cushing's Syndrome, but needs screening to
exclude the diagnosis, 1mg overnight dexamethasone testing may be
preferable, due to the higher sensitivity of the test.
To Know More About Current Research in Diabetes & Obesity
Journal Please click on:
https://juniperpublishers.com/crdoj/index.php
https://juniperpublishers.com/crdoj/index.php


Comments
Post a Comment